Best Beginner Exercises for Healing Your Colles’ Fracture Ball squeezes Get a squishy stress ball and hold it in your hand Squeeze it (without pain) and hold for 5-10 seconds. Repeat 10 times. Do 3-5 times per day. Wrist flexion and extension range of motion Support your forearm, and bend your wrist up and down as far as you can (pain-free).
Full Answer
How long does it take for range-of-motion to return after injury?
Nov 11, 2011 · Exercises to improve range of motion and strength may also be started. Particular focus should be placed on the fractured area and the joints around the fracture. If you broke a bone near your elbow, mobility exercises should be included for your elbow, wrist, and shoulder.
How long does it take to recover from clavicle fracture rehabilitation?
Both groups began with gentle active range of motion at three to five days postoperatively. At two weeks, the accelerated group initiated wrist/forearm passive range of motion and strengthening exercises, whereas the standard group initiated passive range of motion and strengthening at six weeks postoperatively.
What are range-of-motion exercises for a shoulder fracture?
to 14 days with supervised passive range and active range of motion (PROM and AROM) with physical therapy.6,14 Radiographs should also be taken at 2 to 3 weeks intervals to check for fracture displacement.6,14,22 REHABILITATION GUIDELINES Rehabilitation guidelines for various PHF patterns are lacking in the literature. Following the rules of bone healing
What does physical therapy and rehab entail after a fracture?
Sep 19, 2021 · Grip And Range Of Motion Exercises. With your average non-complicated wrist fracture, gentle introduction to gripping and range of motion exercises in every direction is exactly what your wrist wants and needs. Below you will find multiple videos to help get your wrist and hand moving again!
What are active ROM exercises?
Active ROM is the movement of a joint provided entirely by the individual performing the exercise. Active ROM is done without an outside force aiding in the movement. Active assisted ROM involves the joint receiving partial assistance from an outside force.
What are the 3 types of range of motion?
There are three basic types of range of motion: passive, active-assistive and active, defined by the whether, and to what degree, the patient can move the joint voluntarily.
What are the 4 types of range of motion?
How Is Range of Motion Measured?Passive Range of Motion.Active-Assistive Range of Motion.Active Range of Motion.Jun 19, 2020
What is active-assistive range of motion?
Active assisted range of motion Active assist range of motion is described as a joint receiving partial assistance from an outside force. This range of motion may result from the majority of motion applied by an exerciser or by the person or persons assisting the individual.
Why is active range of motion important?
Active range of motion helps build muscle strength. This means improving the fitness of the muscles and joints at the same time. If a person is able to fully move the limb, active exercises are better to improve toning and strength. Passive ROM only keeps joints flexible.
What is active and passive range of motion?
21.2. Passive range of motion can be defined as what is achieved when an outside force, such as a therapist, causes movement of a joint. It is usually the maximum range of motion. Active range of motion is what can be achieved when opposing muscles contract and relax, resulting in joint movement.
What are the 5 types of motion?
There are different types of motion: translational, rotational, periodic, and non periodic motion.Nov 18, 2019
What are active and passive exercises?
Passive exercises are used to prevent stiffness and regain range of motion in muscles, whereas active exercises help strengthen the communication between the brain and body for increased movement.Jan 15, 2017
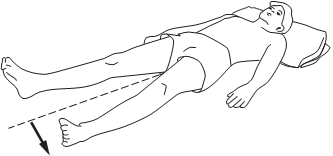
What to do after a fractured leg?
If you break your leg or ankle, a physical therapist may instruct you in how to walk with an assistive device, like a cane or crutches. This includes how to use the device to walk up and down stairs or to get into and out of a car.
How long does it take for a fracture to heal?
In general, a fracture should be healed by about eight weeks. 8 Your rehab timeline will depend on the type of fracture, your age, and other factors. Your physical therapist should be able to give you an idea of how long your rehab program is expected to last.
What to wear if you fracture your shoulder?
If you fracture your shoulder or arm, you may be required to wear a sling to keep the arm immobilized. Check with your doctor to ensure that you understand what is expected of you in regard to immobilization. 2 . How to Take Care of a Cast.
How to reduce scar adhesions?
Scar massage and mobilization can help reduce scar adhesions and improve mobility around the scar. 5 . Exercises to improve range of motion and strength may also be started. Particular focus should be placed on the fractured area and the joints around the fracture.
What is the procedure called when you have a fractured bone?
For more serious fractures, a surgical procedure called an open reduction internal fixation (ORIF) may be necessary to make sure that all the bone pieces are in the correct place and healing can occur. 1 . Often after fracture, the bone needs to be stabilized or immobilized to ensure proper healing. This is usually accomplished using a cast.
What happens after a broken bone?
After a fracture, your bone will be set, or reduced, by a doctor. Reduction of the bone can be done manually.
What to do if you have a broken leg?
If you have fractured your leg, your physical therapist can help you improve walking and help decide if you should walk with a walker, crutches, quad cane, or standard cane. If you have fractured an arm or shoulder, functional activities that focus on reaching and grasping may be included. 3 .
How long does it take to get back to range of motion after a sprain?
This can lead to joint stiffness and loss of range of motion. Range-of-motion exercises often begin six to eight weeks after your injury, according to the University of Utah Health Care. However, certain movements might be restricted longer — especially if you've had surgery. Advertisement.
How to move shoulder with stick?
Dowel shoulder mobility exercises, as recommended by Princeton University Athletic Medicine, are initiated when you are allowed to move your injured shoulder with the help of your other arm. These exercises use a dowel, or stick, to help movement. Perform each exercise 10 times, working up to three sets in a row.
How to do a dowel with your arm?
Lift your arm out to the side while pushing the opposite end of the dowel with your unaffected arm. Your arm should be parallel to the ground throughout the movement. This exercise can also be progressed to a standing position. Move #3: External Rotation. Sit up straight with your elbows by your side.
What is the socket in your shoulder?
The socket is deep in your shoulder joint and relatively well protected. When a shoulder fracture occurs, it most often affects the humerus. However, fractured shoulder recovery exercises can help. Advertisement.
How to do a dowel exercise?
Perform each exercise 10 times, working up to three sets in a row. Hold each position for two to three seconds, then slowly return to the starting position. Move #1: Flexion. Lie on your back holding the dowel with your hands slightly wider than shoulder-width apart. Begin with the dowel resting across your hips.
What is the ball and socket joint?
This ball and socket joint is formed by your humerus (upper arm bone) and scapula (shoulder blade).
How to get rid of a swollen arm?
Sit up straight with your elbows by your side. Hold one end of the dowel in your hand on the affected side. Grasp the middle of the dowel with your other hand. Keeping your elbow tight against your side, rotate your fore arm away from your body. Push the dowel with the opposite arm to assist your movement.
What is the goal of physical therapy after an elbow fracture?
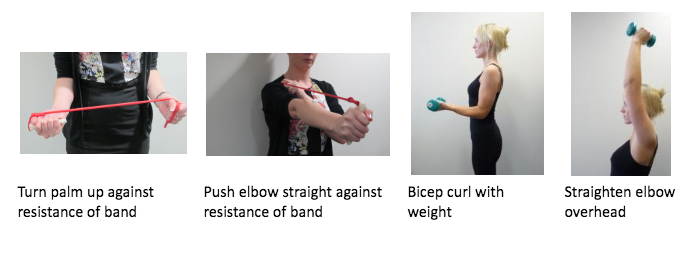
Some impairments that you may work on in physical therapy may include: Range of motion: One of the main goals of physical therapy after an elbow fracture is to restore normal range of motion to the elbow. The elbow is a complex joint that allows you to bend your arm or turn your hand over.
What to do after a fractured elbow?
After a diagnosis of a fractured elbow is made, your doctor will reduce the fracture. This is the process where your elbow bones are put in the correct position so that optimal healing can take place. Reduction of a fractured elbow can be done manually.
How to tell if your elbow is broken?
Common signs of a broken elbow include: 1 Pain in the elbow, upper arm, or forearm 2 Swelling around the elbow 3 Bruising or discoloration around the elbow 4 Loss of motion around the elbow or forearm 5 Deformity (such as a lump or bump) near the elbow or arm
What is the bone that meets the bones of the forearm called?
An elbow fracture also can limit your ability to work, perform household chores, or participate in recreational activities. The elbow is a joint where the arm bone (humerus) meets the bones of the forearm (radius and ulna). The bony end of the ulna is called the olecranon process.
What does it mean when your elbow hurts?
Pain in the elbow, upper arm, or forearm. Swelling around the elbow. Bruising or discoloration around the elbow. Loss of motion around the elbow or forearm. Deformity (such as a lump or bump) near the elbow or arm. If you suspect you have suffered an elbow fracture, you must seek medical attention immediately.
How to heal elbow fracture?
Be sure to discuss with your doctor what outcome is expected in your specific situation. Physical therapy after an elbow fracture can be helpful in safely starting early mobility. It can also help you restore normal strength and function in your arm while helping to manage the pain and swelling that you may experience.
What is the elbow joint?
The elbow is a complex joint that allows you to bend your arm or turn your hand over. Working on restoring full range of motion of the elbow and forearm is paramount to regaining normal use of your arm. If your range of motion loss is severe, your physical therapist may have you wear a dynamic splint.
When will the incidence of proximal humerus triple?
Fractures of the proximal humerus are increasing, with theexpectation that the incidence will triple by 2030 related to ouraging population.6,7Despite the incidence of falls in men beingmore frequent than in women among community-dwelling
What is closed reduction and percutaneous pinning?
Closed reduction and percutaneous pinning is a minimallyinvasive technique that has been primarily indicated for 2-partfractures with minimal comminution and 3- and 4-part valgusimpacted fractures with minimal comminution of the tuber-osities.6Theo retically, this technique is soft-tissue sparing andmay reduce vascular/healing complications.5,6,14 Good out-comes can be achieved 70% of the time in 2-part fracturepatterns.14 Comparison of percutaneous techniques in allfracture patterns revealed that 4-part fractures had the poorestresults. Reported complications of this technique include pin-track infections, avascular necrosis of the humeral head, andpin migration with resultant loss of reduction.14In a study by Boons et al,10hemiarthroplasty was com-pared with nonoperative treatment in a group of 50 elderlypatients with 4-part humeral fractures. There were no differ-ences in the Constant-Murley scores between the 2 groups atthe 3- and 12-month follow-up. The nonoperatively treated andhemiarthroplasty groups had an improved Constant-Murleyscores at 12 months compared with 3 months postoperatively.Forward flexion and abduction were better at 3 months afternonoperative treatment but no longer at 12 months. Also withno difference at 12 months, the mean values for pain asmeasured on a Visual Analog Scale at 3 months were better inthe hemiarthroplasty group than in the nonoperative group.Reverse shoulder arthroplasty (RSA) has recently beenadvocated for the treatment of 4-part fractures. The thought isthat the RSA does not depend on the rotator cuff for elevation,and therefore is not dependant on tuberosity union.15RSAholds a number of theoretic advantages over hemiarthroplastyin the management of these fractures.16Functional outcomesseem to depend less on tuberosity healing and rotator cuffintegrity and patients have been observed to recover morequickly, with less requirement of careful protection and reha-bilitation than hemiarthroplasty.16The overall complicationrate of RSA for fracture is 13% to 28%, which is similar to therate of RSA for rotator cuff tear arthropathy.15Garrigues et al17performed a retrospective review of 23patients comparing reverse total shoulder arthroplasties andhemiarthroplasty treatment. This study showed a statisticallysignificant superiority of reverse total should arthroplastyversus hemiarthroplasty for fracture. The mean AmericanShoulder and Elbow Society (ASES), University of PennsylvaniaShoulder Score (Penn), and Single Assessment Numeric Evalu-ation (SANE) Scores showed a significant difference given thesmall number of patients included in the study and mean activeforward elevation after reverse total shoulder arthroplasty was122 degrees compared with a hemiarthroplasty mean of 90degrees. Another study comparing RSA with hemiarthroplastyby Boyle et al16 found no statistical difference in OxfordShoulder Score at 6 months between groups. However, the RSAgroup displayed a superior Oxford Shoulder Score at 5 yearscompared with the hemiarthroplasty group.
What is a PHF?
humerus fractures ( PHFs) are the third mostcommon fracture type in individuals older than 65 years,after distal radius and proximal femur fractures.1They accountfor approximately 5% of all fractures and have a substantialimpact on personal function and the overall function of anindividual.2,3Indications to treat a PHF nonoperatively, with surgicalfixation, or with arthroplasty, are still evolving. For the most part,patients with a PHF can be treated successfully without operativeintervention. Approximately 80% of PHFs are minimally dis-placed low-energy injuries and are at low risk for future dis-placement, nonunion, or avascular necrosis.4,5For fractures withsevere displacement, the decision for the type of treatmentbecomes more difficult. Indications for treatment are typicallybased on the patient’s age and activity level, as well as radio-graphs and fracture patterns to assess the risk of vascular injuryand potential avascular necrosis as well as assessing the severityof osteoporosis, which can affect the success of the operation.5Physical therapy plays a significant role in the outcome of anindividual’s function after a PHF. Whether the choice is made tohave surgical intervention or nonoperative care, a patient will beseen in physical therapy for a variety of strategies and progressionsto return them to their optimal level of function. To date, nocurrent literature exist specifying rehabilitation guidelines forconservative and surgical interventions. We will introduce con-servative management guidelines and outline current rehabilitationphases for postoperative management.
How long does it take for a wrist fracture to heal?
Wrist fractures are unfortunately a slow recovery. It can take a really long time, even up to a year, for your wrist to feel back to 100% normal like it did prior to the injury. This is especially true in regards to grip strength, being able to support all of your weight through that wrist and hand, and doing everyday activities using your wrist and hand. The bottom line is you have to be patient, remind yourself of how far you’ve come compared to day 1 of having your cast on. If you continue to have significant limitations and pain with your wrist, it may be in your best interest to seek help from a physical therapist or certified wrist and hand specialist.
How long do you have to be in a cast to get a bone out?
Next thing you know you’re in a cast for 4-6 weeks. Time goes by, you see the doctor and he says the bone is healed, you’re good to go! You get the cast removed, but you realize your wrist and hand look shriveled up and tiny compared to the other side.
What is a broken wrist?
A broken wrist, also referred to as a wrist fracture, is typically a break in the distal radius bone, which is one of the bones in your forearm on the thumb side. Wrist fractures typically occur from falling due to the natural reaction to try and break the fall by reaching out and landing on the hand. As you can see above, the more common wrist ...
What bone is tender to touch?
Thus if you have a very swollen wrist, a visible deformity of your wrist, and it is tender to touch on the inside of your wrist at the distal radius bone, it is likely in your best interest to seek medical attention and get x-rays to confirm if you have a wrist fracture or not.
What is the most common wrist fracture?
As you can see above, the more common wrist fracture to occur from a FOOSH (Falling Onto An Outstretched Hand) injury is termed a Colle’s Fracture. From the picture above, you can also see that Smith’s Fracture also can occur which results in an inward motion of the wrist, but this is less common than the Colle’s Fracture.
How to move a finger that is not affected?
Place the hand with the affected finger flat on a table, palm up. With your other hand, press down on the fingers that are not affected. Your affected finger will be free to move.
How to do slide 9 of 9?
slide 9 of 9, Towel grab, Fold a small towel in half, and lay it flat on a table. Put your hand flat on the towel, palm down. Grab the towel, and scrunch it toward you until your hand is in a fist. Slowly straighten your fingers to push the towel back so it is flat on the table again. Repeat 8 to 12 times.
How to get a swollen finger out of your hand?
Place your good hand on a table, palm up. Put your hand with the affected finger on top of your good hand. Use the thumb and fingers of your good hand to grasp below the middle joint of your affected finger. Bend and then straighten the last two joints of your affected finger. Repeat 8 to 12 times.
How to get a hook out of your hand?
Slowly uncurl the joints of your hand with the affected finger where your fingers connect to your hand so that only the top two joints of your fingers are bent. Your fingers will look like a hook. Move back to your starting position, with your fingers wrapped around your good thumb. Repeat 8 to 12 times.
How to do MP extension?
MP extension. Place your good hand on a table, palm up. Put your hand with the affected finger on top of your good hand with your fingers wrapped around the thumb of your good hand like you are making a fist. Slowly uncurl the joints of your hand with the affected finger where your fingers connect to your hand so that only the top two joints ...
How to do dip flexion?
slide 3 of 9, DIP flexion, With your good hand, grasp your affected finger. Your thumb will be on the top side of your finger just below the joint that is closest to your fingernail. Slowly bend your affected finger only at the joint closest to your fingernail. Hold for about 6 seconds.
How to make a fist?
Make a fist by bending your knuckles. Your thumb can gently rest against your index (pointing) finger. Unwind your fingers slightly so that your fingertips can touch the base of your palm. Your thumb can rest against your index finger . Move back to your starting position, with your fingers and thumb pointing up.
