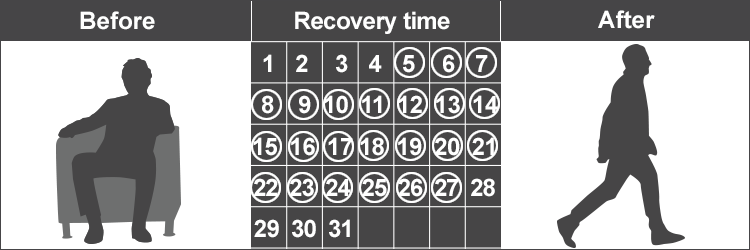
To benefit from intense therapy, the patient must be able to devote three hours each day, five to six days per week. Patients may require treatment from two or more different therapeutic fields. It is recommended that patients continue in rehabilitation for at least five days.
How many hours a day is intensive rehabilitation?
You must pay the inpatient hospital deductible for each benefit period. There's no limit to the number of benefit periods. Days 1-60: $1,556 deductible.*. Days 61-90: $389 coinsurance each day. Days 91 and beyond: $778 coinsurance per each “lifetime reserve day” after day 90 for each benefit period (up to a maximum of 60 reserve days over ...
How long does Medicare pay for inpatient rehab?
Unfortunately, there is no clear-cut answer as to how long an inpatient rehab program lasts. This is largely due to addiction being unique to every individual. However, typical programs range …
What are the costs for a rehab stay?
• The patient can actively participate in and benefit from intensive therapy that most typically consists of three hours of therapy a day at least five days a week. • The patient is sufficiently stable at the time of admission to actively participate in the intensive rehabilitation program.
When will I be admitted to an inpatient rehabilitation facility?
In order to engage in an intense therapy program, the patient must be able to devote 3 hours per day, 5 to 6 days per week. Patients may require treatment from two or more different fields. Patients are required to stay in rehab for a minimum of five days.

Where does rehabilitation take place?
Rehabilitation may take place in a special section of the hospital, in a skilled nursing facility, or in a separate rehabilitation facility. Although Medicare covers your care during rehabilitation, it’s not intended to be long-term care. You can learn more about Medicare and long-term care facilities here.
What to do if you have a sudden illness?
Though you don’t always have advance notice with a sudden illness or injury, it’s always a good idea to talk with your healthcare team about Medicare coverage before a procedure or inpatient stay, if you can.
Does Medicare cover rehab?
Medicare Part A covers your inpatient care in a rehabilitation facility as long as your doctor deems it medically necessary. In addition, you must receive care in a facility that’s Medicare-approved. Depending on where you receive your inpatient rehab therapy, you may need to have a qualifying 3-day hospital stay before your rehab admission.
Does Medigap cover coinsurance?
Costs with Medigap. Adding Medigap (Medicare supplement) coverage could help you pay your coinsurance and deductible costs. Some Medigap plans also offer additional lifetime reserve days (up to 365 extra days). You can search for plans in your area and compare coverage using Medicare’s plan finder tool.
Does Medicare cover knee replacement surgery?
The 3-day rule does not apply for these procedures, and Medicare will cover your inpatient rehabilitation after the surgery. These procedures can be found on Medicare’s inpatient only list. In 2018, Medicare removed total knee replacements from the inpatient only list.
Does Medicare cover inpatient rehabilitation?
Medicare covers your treatment in an inpatient rehabilitation facility as long as you meet certain guidelines.
How long does it take to get into drug rehab?
Drug Rehab Treatment Information. By Length Care. Most rehab programs range from 28 days to 90 days, depending on your needs and what you want from your treatment program. However, programs vary greatly and you can find shorter and longer stays, as well as both outpatient and inpatient residential treatment programs.
What is rehab program?
Some rehab programs study the outcomes of their patients and can provide this information to prospective patients. They may also publish this information online. You can also read reviews of programs to get a sense of whether they’re actually helping people.
What is MAT in medical?
Medication-assisted treatment (MAT) involves the use of medications, such as methadone, combined with counseling to treat opioid and alcohol addictions. 4. Mental health services. Medical care, when needed. Participation in 12-step recovery groups, such as Alcoholics Anonymous (AA). Career development training.
How long does it take to recover from a drug addiction?
60 days. 90 days. Long-term recovery (90-120 days and beyond). The actual amount of time you spend in treatment will depend on a number of things, including: Severity of addiction. Need for detox. Insurance. If no insurance, ability to self-pay. Medical/mental health issues that need treatment.
What is drug monitoring?
Monitoring drug use during treatment. Testing patients for diseases and other conditions from drug use, such as HIV/AIDS, hepatitis, and tuberculosis. You may want to evaluate a program you’re interested in based on how well they follow these guidelines.
How long does methadone stay in your system?
NIDA recommends even longer-term treatment to maintain sobriety. 1. People who take methadone for opioid addiction may be on the medication for at least a year. Many continue to take it for many years. 1. For many people, recovery is a long-term process.
How to deal with addiction?
Take down your medical history. Evaluate the nature and severity of your addiction, as well as your mental state. Recommend an appropriate treatment plan for you. The treatment plan will include goals for your treatment and a discharge plan.
How long does Medicare cover SNF?
After day 100 of an inpatient SNF stay, you are responsible for all costs. Medicare Part A will also cover 90 days of inpatient hospital rehab with some coinsurance costs after you meet your Part A deductible. Beginning on day 91, you will begin to tap into your “lifetime reserve days.".
How much is Medicare Part A deductible for 2021?
In 2021, the Medicare Part A deductible is $1,484 per benefit period. A benefit period begins the day you are admitted to the hospital. Once you have reached the deductible, Medicare will then cover your stay in full for the first 60 days. You could potentially experience more than one benefit period in a year.
Does Medicare cover rehab?
Learn how inpatient and outpatient rehab and therapy can be covered by Medicare. Medicare Part A (inpatient hospital insurance) and Part B (medical insurance) may both cover certain rehabilitation services in different ways.
Does Medicare cover outpatient treatment?
Medicare Part B may cover outpatient treatment services as part of a partial hospitalization program (PHP), if your doctor certifies that you need at least 20 hours of therapeutic services per week.
Is Medicare Advantage the same as Original Medicare?
Medicare Advantage plans are required to provide the same benefits as Original Medicare. Many of these privately sold plans may also offer additional benefits not covered by Original Medicare, such as prescription drug coverage.
Who is Christian Worstell?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. .. Read full bio
What is the 60% rule for rehabilitation?
An inpatient rehabilitation facility (IRF) is eligible for payment as an IRF under the Center for Medicare and Medicaid Services (CMS) prospective payment system if it complies with a number of regulations set forth by CMS. Sixty percent of patients admitted to the unit must have 1 of 13 conditions: stroke, spinal cord injury, congenital deformity, amputation, major multiple trauma, fracture of the hip, brain injury, burns, active polyarthritis, systemic vasculitis with joint involvement, specified neurologic conditions, severe or advanced osteoarthritis, knee or hip replacement (if bilateral, body mass index >50, or age 85). This is known as the 60% rule. The patients must be offered an intensive multidisciplinary rehabilitation program. They should attend 3 hours of therapy in 5 of 7 consecutive days. They may attend 15 hours (900 minutes) of therapy in 7 days if there is a reason (such as low endurance) why they cannot attend therapy 3 hours per day in 5 of 7 days (3-hour requirement). The therapies included in the rule are physical therapy (PT), occupational therapy (OT), speech and language pathology (SLP), and orthotic and prosthetic services. The patient must be cared for by nurses with specialized training or experience in rehabilitation services and must be seen by a physician with specialized training in rehabilitation at least 3 times per week. The patient must have a case manager or social worker. There must be an interdisciplinary team conference led by the physician at least once a week. At the time of admission, there must be the expectation that the patient can benefit from therapy. There must be daily notes and team conference notes that provide evidence that the patient's level of function is improving. [1,2]
Why is exercise important in medicine?
Exercise is important in improving strength, endurance, coordination, and the ability to perform functional tasks. [10] .
How long does Medicare cover inpatient rehab?
Medicare covers inpatient rehab in a skilled nursing facility – also known as an SNF – for up to 100 days. Rehab in an SNF may be needed after an injury or procedure, like a hip or knee replacement.
What is an inpatient rehab facility?
An inpatient rehabilitation facility (inpatient “rehab” facility or IRF) Acute care rehabilitation center. Rehabilitation hospital. For inpatient rehab care to be covered, your doctor needs to affirm the following are true for your medical condition: 1. It requires intensive rehab.
What is Medicare Part A?
Published by: Medicare Made Clear. Medicare Part A covers medically necessary inpatient rehab (rehabilitation) care , which can help when you’re recovering from serious injuries, surgery or an illness. Inpatient rehab care may be provided in of the following facilities: A skilled nursing facility.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
How many reserve days can you use for Medicare?
You may use up to 60 lifetime reserve days at a per-day charge set by Medicare for days 91–150 in a benefit period. You pay 100 percent of the cost for day 150 and beyond in a benefit period. Your inpatient rehab coverage and costs may be different with a Medicare Advantage plan, and some costs may be covered if you have a Medicare supplement plan. ...
Does Medicare cover speech therapy?
Medicare will cover your rehab services (physical therapy, occupational therapy and speech-language pathology), a semi-private room, your meals, nursing services, medications and other hospital services and supplies received during your stay.
What is individualized overall plan of care?
The individualized overall plan of care is synthesized by the rehabilitation physician from the preadmission screening, post-admission physician evaluation, and information garnered from the assessments of all disciplines involved in treating the patient. The individualized overall plan of care must:
What is an IRF in nursing?
Admission to an IRF is appropriate for patients with complex nursing, medical management, and rehabilitative needs.
What is CERT in Medicare?
This fact sheet describes common Comprehensive Error Rate Testing (CERT) Program errors related to inpatient rehabilitation services and provides information on the documentation needed to support a claim submitted to Medicare for inpatient rehabilitation services.
What is the purpose of a post-admission physician evaluation?
The purpose of the post-admission physician evaluation is to document the patient’s status on admission to the IRF, compare it to that noted in the preadmission screening documentation, and begin development of the patient’s expected course of treatment that will be completed with input from all of the interdisciplinary team members in the overall plan of care. A dated, timed, and authenticated post-admission physician evaluation must be retained in the patient’s IRF medical record. The post-admission physician evaluation must:
What is an IRF PAI?
The IRF-PAI gathers data to determine the payment for each Medicare Part A FFS patient admitted to an IRF. The IRF-PAI form must be included in the patient’s IRF medical record in either electronic or paper format.
Who generates admission orders?
Admission orders must be generated by a physician at the time of admission. Any licensed physician may generate the admission order. Physician extenders, working in collaboration with the physician, may also generate the admission order.