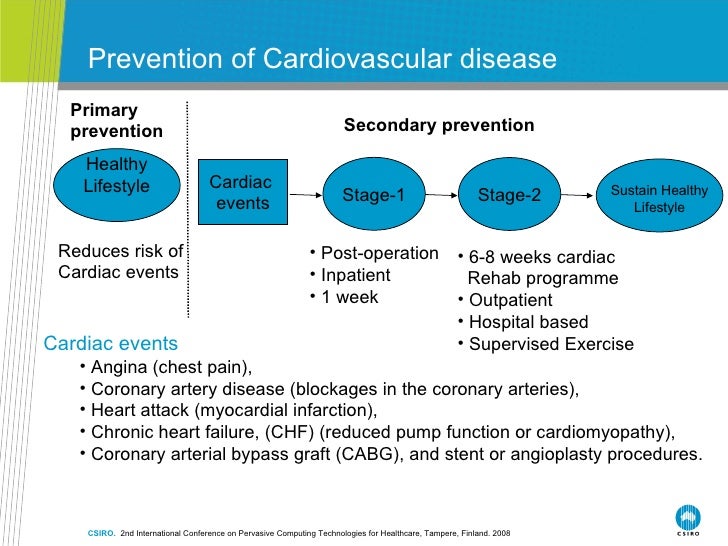
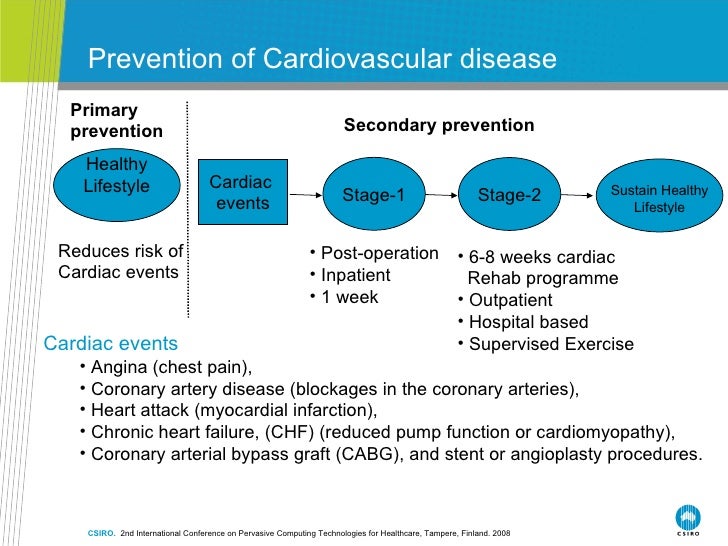
Is cardiac rehabilitation relevant after an mi?
Mar 04, 2018 · Cardiac rehabilitation seemingly benefits patients with coronary heart disease and those with heart failure in terms of physical, mental, cognitive, and social function; and a reduction in morbidity, mortality, and healthcare costs The following ICD-9 Diagnosis codes will allow payment for Cardiac Rehab Services. Cardiac rehabilitation is a comprehensive intervention …
Is cardiac rehabilitation safe for older people?
Feb 12, 2019 · Current cardiac rehabilitation recommendations for post‐myocardial infarction/revascularisation, heart failure and heart valve replacement patients recommend that, in addition to exercise training, psychosocial or educational support, or both, should be offered (Piepoli 2010); so‐called 'comprehensive cardiac rehabilitation'. However, as with exercise …
How should cardiologists support cardiac rehabilitation programs?
Rehabilitation of patients with cardiac pacemakers (CP) or implantable cardioverter defibrillators (ICD) comprises secondary prevention of underlying cardiac disease, conditioning training activities and psychological education and includes furthermore the assessment of aggregate function, detection of any device malfunction as well as the return to work efforts.
What is the ICD 10 code for cardiac rehabilitation?
The average duration of exercise-based cardiac rehabilitation (CR) was 9.6 weeks. Ten ICD therapies (seven shocks) were reported in the 834 patients with ICD during ET. Between exercise sessions and during follow up 182 events were recorded including 166 shocks. Three studies (2 randomized) showed that the control group representing sedentary patients were more prone …
When do you start cardiac rehab after pacemaker?
Cardiac rehab involves in-person visits, typically three times a week, for 12 weeks. It usually starts several weeks after hospital discharge. Your team will check on your overall health as well as your specific heart condition. They will come up with an exercise and eating plan that keeps your limitations in mind.Oct 20, 2021
When should cardiac rehab begin?
Cardiac rehabilitation may start while you are still in the hospital or right after you leave the hospital. Cardiac rehabilitation programs usually last about 3 months but can range anywhere from 2 to 8 months. Talk to your doctor about cardiac rehabilitation.
What diagnosis qualifies for cardiac rehab?
Cardiac rehabilitation programs are appropriate for patients who have had a heart attack; for people who have undergone angioplasty or stenting, open-heart surgery, such as coronary artery bypass surgery, valve replacement or heart transplant; and for people with a diagnosis of angina or heart failure.Nov 4, 2014
Does a pacemaker qualify you for cardiac rehab?
Procedures and surgeries include heart transplants, percutaneous coronary intervention, coronary artery bypass graft, and heart valve replacement. Those who have a pacemaker or implantable cardioverter defibrillator are also candidates for cardiac rehab.Nov 5, 2014
When does the Phase 1 of cardiac rehabilitation begin?
Phase 1: Acute, In Hospital Patient Period Patients with acute heart conditions, such as those recovering from heart surgery or a heart attack, may be referred to a cardiac rehab team while still in hospital. This phase will likely last between 2 and 5 days, depending on your physical condition.May 14, 2019
What are the 4 phases of cardiac rehab?
Once significant healing has taken place, you may be discharged home to begin phase two cardiac rehab.The Subacute Phase. Once you leave the hospital, your cardiac rehabilitation program will continue at an outpatient facility. ... Intensive Outpatient Therapy. ... Independent Ongoing Conditioning.Oct 10, 2021
What ejection fraction qualifies for rehab?
O'Connor and colleagues reported the results of an NHLBI funded, multicenter, randomized controlled trial of medically stable patients “to test the efficacy and safety of exercise training among patients with heart failure.” Inclusion criteria were LVEF ≤ 35% and NYHA class II-IV despite optimal therapy for at least ...
When does cardiac rehab start after CABG?
The earliest rehabilitation is possible in patients following less invasive heart surgery and may start one to two weeks postoperatively.
What are the 3 phases of cardiac rehab?
Comprehensive programPhase 1: Hospitalization. Evaluation, education and rehabilitation efforts begin while you're still in the hospital following a cardiac event.Phase 2: Early outpatient. ... Phase 3: Extended outpatient.Oct 29, 2021
How many cardiac rehab sessions does Medicare allow?
You can receive cardiac rehabilitation care in a hospital outpatient department or at a doctor's office. Medicare covers up to two one-hour sessions per day for up to 36 sessions. These sessions must occur during a 36-week period. If medically necessary, Medicare will cover an additional 36 sessions.
What are the exercises for cardiac rehab?
“Generally, cardiac rehabilitation sessions involve a brief warm-up and stretching period, followed by 30-40 minutes of aerobic exercise. This can involve treadmill, stationary bicycle, elliptical or rowing machines. Sometimes, resistance training is incorporated.Jul 25, 2016
Is cardiac rehab necessary after aortic valve replacement?
Cardiac rehabilitation (CR) is approved by the Centers for Medicare and Medicaid Services for patients who have had heart valve surgery. Analysis of data shows that CR increases exercise capacity and quality of life, and facilitates return to work, with minimal risk of significant adverse effects.
How long should I warm up for ICD?
A sharp spike in heart rate could potentially set off your ICD. Therefore, you should include a low-level 5 to 10 minute warm-up and cool-down phase for aerobic exercise (i.e., walking, cycling) to allow for a slow and steady increase in heart rate. After that, work up to a low to moderate intensity.
What is the exercise prescription for a cardioverter?
The four fundamental components of an exercise prescription are easily remembered by the FITT acronym: Frequency, Intensity, Time (duration), and Type of exercise . So a basic exercise prescription for a person with an implanted cardioverter defibrillator might entail the following:
What is an implanted cardioverter defibrillator?
As stated above, your implanted cardioverter defibrillator is designed to “zap” you back to normal rhythm in the event your heart starts racing or beating erratically. Exercise also causes your heart rate to increase, but this is a normal and expected response. So how does your implantable cardioverter defibrillator tell ...
How to avoid arrhythmias?
Avoid lifting weights so heavy that they leave you grunting, groaning, and gasping for air. This may increase the intrathoracic pressure, forcing your heart to work harder, and consequently set the stage for a possible arrhythmia (and subsequent shock). Rule of thumb: EXHALE ON THE EXERTION. In other words, when the weight is being lifted against gravity, exhale to release that internal pressure.
How does ICD implantation affect your life?
Appropriate exercise specific to ICD implantation can enhance your overall well-being and quality of life. Regular training promotes healthy changes in the muscles and your collective cardiorespiratory (heart and lungs) system which, over time, makes your day to day living much easier.
Where is the implantable cardioverter implanted?
An implantable cardioverter defibrillator is a small, thin, battery-powered device implanted just under the skin in the chest region and is designed to deliver a shock to restore normal cardiac rhythm in those at risk for sudden cardiac death due to malignant arrhythmias like ventricular fibrillation or tachycardia.
How to get a good heart rate?
Try to exercise at a “moderate” level, somewhere in the range of 4 to 6, and adjust based upon your body’s response. Also take note of your heart rate when you’re at a moderate workload. Though you may be on beta-blockers, this will reflect your individual response to exercise and can help serve as a guide.
