How to write a patient’s discharge from A&E?
who have completed Optima 101 training. This guide is designed as a “quick reference guide” to assist you while performing your daily tasks in Optima’s Care Operations Management. The Participant Guide provides simple, step-by-step instructions for completing tasks. We recommend that you use this guide in conjunction with the short micro-
What is a discharge summary for outpatient therapy?
Rehab Optima Documentation: Discharge Summary Rehab Optima Training Videos for Documentation Questions, please email RO@bigstonetherapies.com, or call Nicole at (320) 839.4082 Rehab Optima on Vimeo
How long does it take to get Optima therapy for SNFS?
He or she authorizes (approves) the rehab discharge. A nurse. Often this is the head nurse of your family member’s unit, who will coordinate any education regarding medications and other nursing issues. A social worker. This person coordinates the discharge, making sure that everything happens when it should. He or she also takes care of many details about rehab discharge.
What should be included in a discharge letter?
May 12, 2015 · Are you a Rehab Optima user looking to refresh your knowledge or learn how the system handles intakes and discharges? Our next Lunch & Learn will provide an overview of the intake, re-intake, and discharge processes, as well as tips regarding how you can make them as efficient as possible. Title: Back to Basics: Intake/Re-Intake/Discharge
What is Rehab Optima called now?
What is a ten document on Optima?
Is Rehab Optima easy to use?
Is Rehab Optima web based?
How to plan for discharge?
good way to start planning for discharge is by asking the doctor how long your family member is likely to be in the rehabilitation (“rehab” or “subacute”) facility. The doctor or physical therapist may have a general idea when the admission begins. But they may not know how long your family member will continue to improve, which is a requirement under Medicare and other insurance. Once improvement stops or significantly slows, insurance will discontinue payment, which may make discharge very rapid. Insurance may have other restrictions as well.
Can a family member eat milk?
member can or cannot eat. This might include specific foods such as milk or meat, or general types of food, such as very soft food or liquids. If your family member needs any special foods, try to buy them before discharge when it is easier to shop.
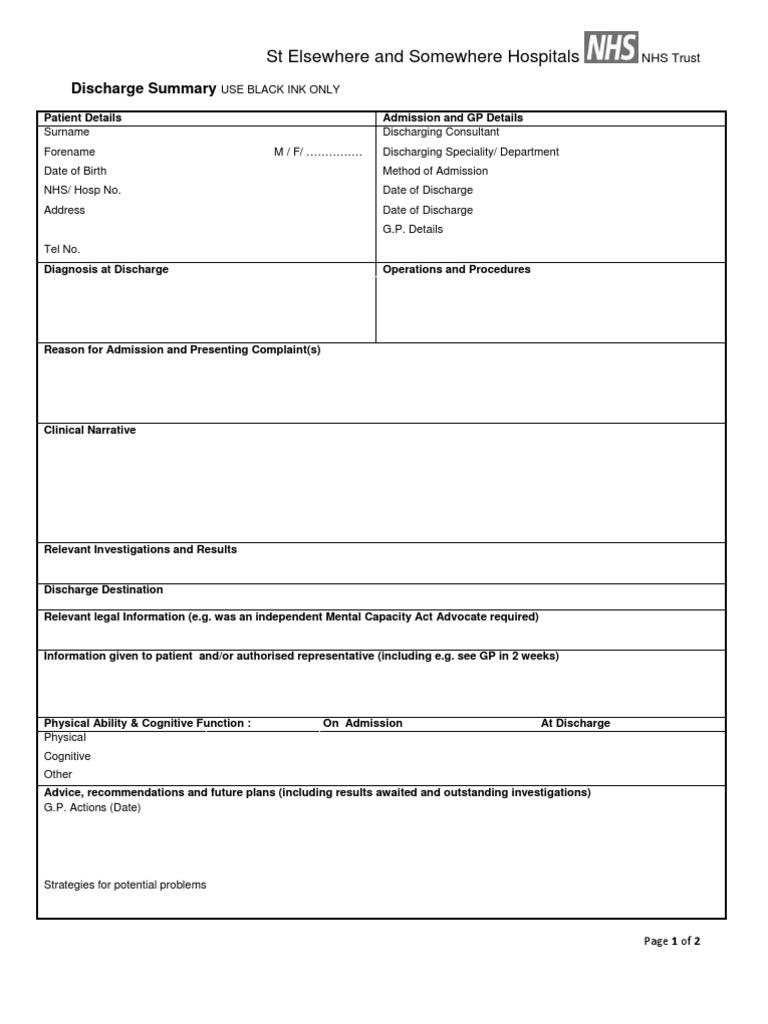
What is discharge summary?
Functionally, a discharge summary (a.k.a. discharge note) is a progress note that covers the reporting period from the last progress report to the date of discharge. The discharge summary is required for each episode of outpatient therapy treatment.
What information should a therapist base on a discharge?
In the case of an unanticipated discharge (e.g., the patient stops showing up for therapy or self-discharges), the therapist may base any treatment or goal information on the previous treatment notes or the verbal reports of a PTA or other clinician. Furthermore, as this CMS document explains, “In the case of a discharge anticipated within 3 treatment days of the Progress Report, the clinician may provide objective goals which, when met, will authorize the assistant or qualified personnel to discharge the patient. In that case, the clinician should verify that the services provided prior to discharge continued to require the skills of a therapist, and services were provided or supervised by a clinician.”
What information is needed for physical therapy?
Physical therapists, on the other hand, are solely responsible for noting the following required information: 1 assessment of patient improvement or progress toward each goal; 2 decision regarding continuation of treatment plan; and 3 any changes or additions to the patient’s therapy goals.
What is progress note?
According to Mosby’s medical dictionary, progress notes are “notes made by a nurse, physician, social worker, physical therapist, and other health care professionals that describe the patient’s condition and the treatment given or planned.”.
What is the responsibility of a physical therapist?
Physical therapists, on the other hand, are solely responsible for noting the following required information: assessment of patient improvement or progress toward each goal; decision regarding continuation of treatment plan; and. any changes or additions to the patient’s therapy goals.
Can you complete a progress report prior to a 10th visit?
You can also complete a progress report prior to the tenth visit (for example, if you know you will be unable to assess the patient personally during the tenth visit, you could complete the progress note during the ninth visit). It’s important to note, however, that the reporting period would then reset on the ninth visit, meaning the tenth visit would serve as the first session for the new 10-visit reporting period.
What is discharge summary?
A discharge summary is a clinical report prepared by a health professional at the conclusion of a hospital stay or series of treatments. It is often the primary mode of communication between the hospital care team and aftercare providers.
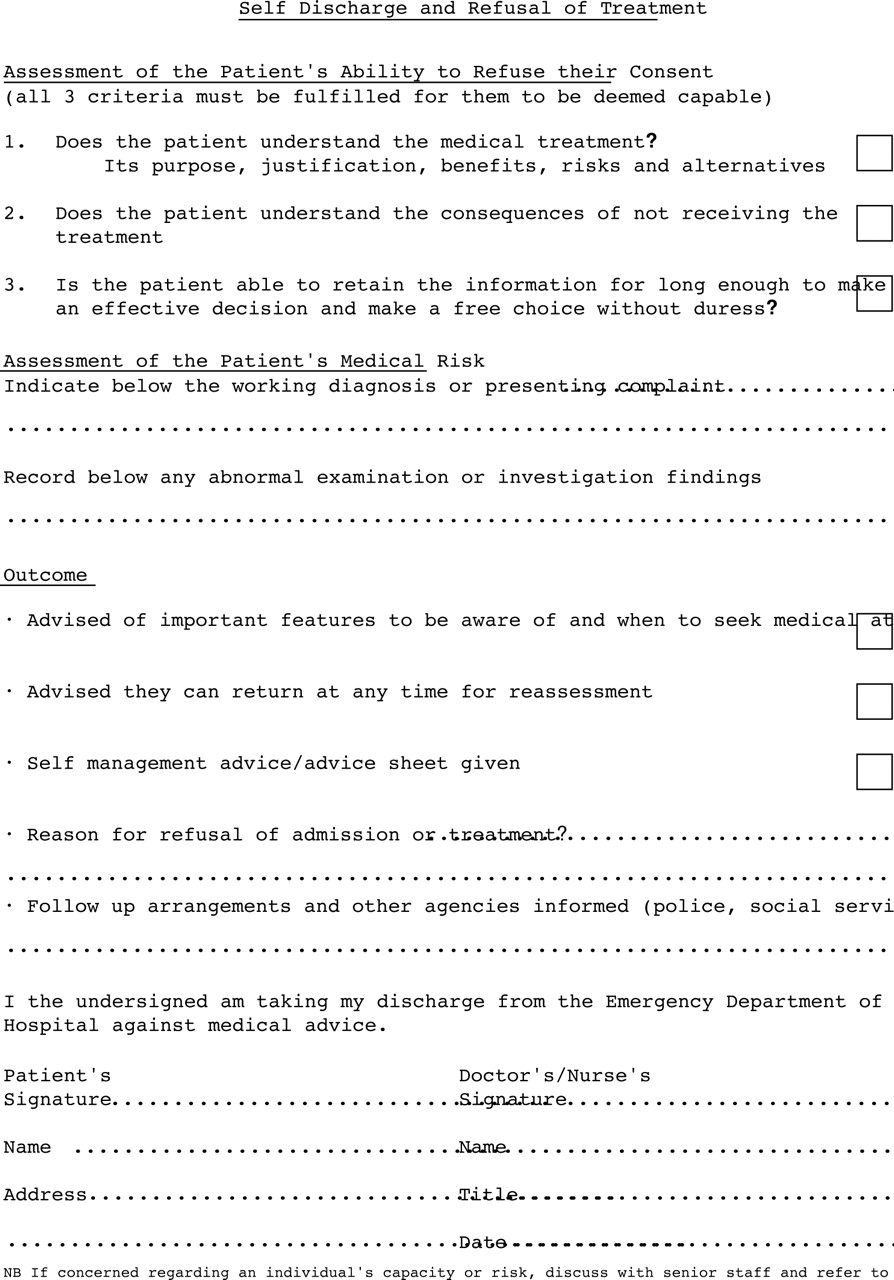
What is advance decision?
Advance decisions about treatment: Whether there are written documents, completed and signed when a person is legally competent, that explains a person’s medical wishes in advance, allowing someone else to make treatment decisions on his/her behalf late in the disease process. Location of these documents.
What is a causal agent?
Causative agent: the agent (food, drug or substances) that caused an allergic reaction or adverse reaction. Description of the reaction: this may include the manifestation (e.g. rash), type of reaction (allergic, adverse, intolerance) and the severity of the reaction.