How to find out if your insurance covers drug rehab?
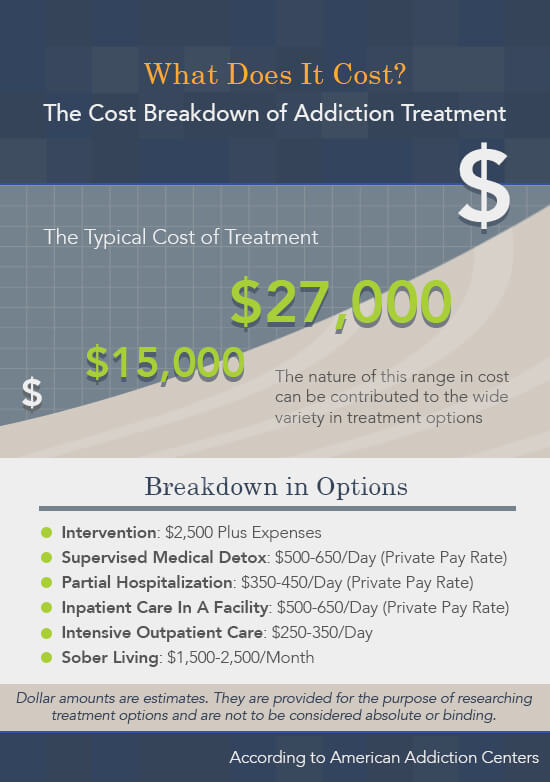
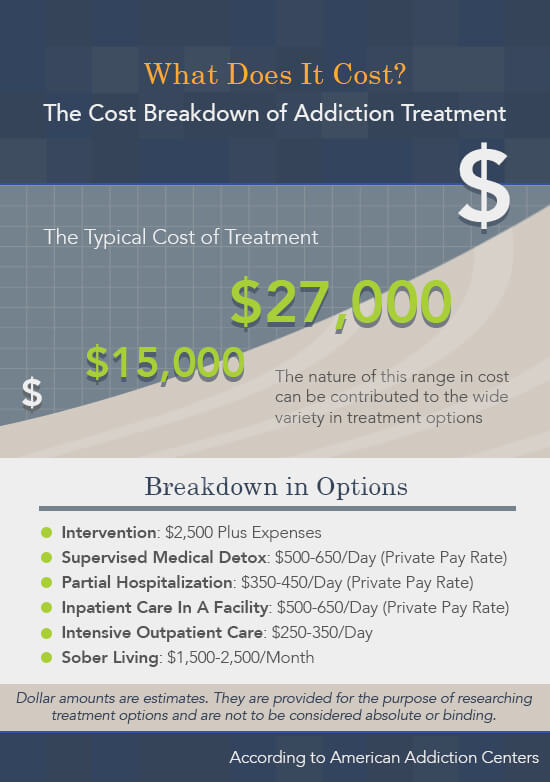
Some recovery options, such as programs from non-profit health centers, are entirely free while luxury centers for celebrities might cost up to $80,000 a month. Most standard drug treatment centers fall somewhere in the middle, from $2,000 to $25,000 a month. The cost varies depending on location, length, and what’s included.
How to get drug rehab coverage from an insurance provider?
Apr 04, 2022 · Health insurance typically covers substance abuse rehabilitation and various forms of mental health treatment. However, the extent to which your insurance will cover drug or alcohol rehab depends upon a variety of factors, including your policy’s particular behavioral health benefits, your rehab treatment provider, your particular needs, and more.
How long does insurance cover drug rehabilitation?
Feb 01, 2019 · Does insurance cover rehab? In short, yes. But not all insurance plans will cover all types of drug and alcohol rehabilitation. Private insurance companies vary significantly in how much addiction treatment coverage they provide. Public insurance programs, such as Medicare and Medicaid, provide coverage.
How to get insurance to pay for drug rehab?
Feb 26, 2020 · Does Insurance Cover Rehab? Insurance typically covers substance abuse treatment, including inpatient services, outpatient services, psychotherapy and counseling. For complete details regarding your coverage, call your insurance provider and ask about mental health and substance abuse treatment coverage.
Does healthcare cover drug overdose?
The quick answer is yes. Life insurance policies do cover drug overdose deaths. It doesn't matter what the substance is or how illegal it is to possess it. Life insurers will pay out the policy's death benefit, even if the insured's death resulted from an overdose of drugs or alcohol.
What do doctors prescribe for drug addicts?
Experts believe that “medication-assisted treatment” with methadone, naltrexone, or suboxone and cognitive behavioral therapy is the best treatment for most patients who have an opioid addiction. Counseling is the most common treatment for addiction to CNS depressants or stimulants.Mar 17, 2022
Does insurance cover alcohol intoxication?
Injuries and illnesses experienced as a result of alcohol or other substance abuse is often excluded in health and medical insurance.Dec 28, 2018
Can you get life insurance on a drug addict?
Insurers will not, in most cases, cover current illicit drug users. If you currently take illicit drugs or abuse therapeutic drugs not prescribed to you, you will likely be immediately denied by a life insurance company.Mar 31, 2021
What are 3 commonly abused prescription drugs?
Three types of drugs are abused most often: • Opioids—prescribed for pain relief • CNS depressants—barbiturates and benzodiazepines prescribed for anxiety or sleep problems (often referred to as sedatives or tranquilizers) • Stimulants—prescribed for attention-deficit hyperactivity disorder (ADHD), the sleep disorder ...
What are the 4 types of drugs?
There are four main groups of drugs, divided according to their major effects, plus a few substances that do not easily fit into any category....What types of drug are there?stimulants (e.g. cocaine)depressants (e.g. alcohol)opium-related painkillers (e.g. heroin)hallucinogens (e.g. LSD)
What are the five stages of intoxication?
Different Stages of Alcohol IntoxicationWhat Is Alcohol Intoxication?The Stages of Alcohol Intoxication.Stage 1: Sobriety, or Subclinical Intoxication.Stage 2: Euphoria.Stage 3: Excitement.Stage 4: Confusion.Stage 5: Stupor.Stage 6: Coma.More items...•Mar 16, 2021
When should a drunk person go to the hospital?
If the person is unconscious, breathing less than eight times a minute or has repeated, uncontrolled vomiting, call 911 immediately. Keep in mind that even when someone is unconscious or has stopped drinking, alcohol continues to be released into the bloodstream and the level of alcohol in the body continues to rise.
What happens if you go to the hospital for drinking?
When to go to the ER Alcohol poisoning is a medical emergency. It can lead to complications such as choking, brain damage, and even death. Prompt medical treatment can help prevent these complications from occurring.Jun 10, 2019
Can I get life insurance if I have been to rehab?
For most life insurance companies, you will need to be drug-free or out of rehab for several years before you'll be offered coverage. If you are currently using illicit drugs you will be denied standard term and permanent life insurance coverage, but might be able to get limited final expense or group insurance.
What reasons will life insurance not pay?
If you die while committing a crime or participating in an illegal activity, the life insurance company can refuse to make a payment. For example, if you are killed while stealing a car, your beneficiary won't be paid.
What percentage of life insurance claims are denied?
Life insurance is nearly always settled as expected. According to the American Council of Life Insurers (ACLI), fewer than one in 200 claims are denied.May 27, 2021
What is the best insurance for substance abuse?
The two most common healthcare plans are HMO and PPO. Substance abuse treatment and recovery may be covered by your insurance provider. Learn more about which plan, HMO or PPO, offers the best coverage: 1 HMO (Health Maintenance Organization) plans allow patients to choose their primary care physician and see that doctor for most of their medical needs. This allows them to form a relationship with a doctor who knows their whole health history. When seeking a specialist or physician outside of the network, a referral is needed by your primary care physician. 1 HMOs have lower or no deductibles and overall coverage is usually a lower cost than PPO. 2 Pros of HMO coverage are for those that are not seeking a specialist and healthcare providers out of their network and paying lower premiums. 2 2 PPO (Preferred Provider Organization) plans allow patients to see healthcare providers in and out of their network without referrals. 3 PPOs can have higher deductibles than those with an HMO plan. 2 One of the pros of PPO coverage is having the option see specialists and other healthcare providers outside of your network without a referral from your primary care physician. 2
How much does it cost to incarcerate an adult?
For example, a PBS report suggests that incarcerating an adult for one year can cost up to $37,000, while providing residential care for addiction costs just $14,600. State-run plans might very well provide robust addiction care for all drugs simply because doing so could keep other costs in line.
What is the one page summary of benefits and therapies?
Under the Affordable Care Act, insurance plans are required to provide a one-page summary of benefits and therapies, along with their fees, per the U.S. Department of Health and Human Services.
How many people didn't have health insurance in 2014?
Now more people than ever before have health insurance. In fact, according to the Kaiser Family Foundation, only 13% of Americans didn’t have health insurance in 2014. Everyone else had the coverage they needed to deal with health problems.
Is health insurance a luxury?
Health insurance was once considered a bit of a luxury. People with tight budgets and low-paying jobs may not have had the extra cash they needed in order to buy expensive health care plans, so they tried to save up enough money to allow them to get care for problems deemed life-threatening. Anything else went unaddressed. Often, that meant addictions went untreated. For people without health insurance, getting medical care for addiction was just too expensive to consider.
Is substance abuse covered by insurance?
Substance abuse treatment and recovery may be covered by your insurance provider. Learn more about which plan, HMO or PPO, offers the best coverage: HMO (Health Maintenance Organization) plans allow patients to choose their primary care physician and see that doctor for most of their medical needs.
Is drug treatment covered by insurance?
Most insurance policies don’t separate drugs into “covered” and “non-covered” categories. If addiction treatments are considered a covered benefit, then care is provided to anyone who has an addiction, regardless of what that addiction is caused by.
What is private insurance?
Private Insurance. Private insurance plans are frequently provided by an employer to cover employees as well as their spouses and dependent children. Private insurance plans are created and maintained by companies including: UnitedHealth. Anthem.
What is Medicaid for low income?
Medicaid is public insurance managed by state and federal government aimed at covering people with low incomes (a percentage above the federal poverty level (FPL) based on your household size) and who are: 8,10. 65 and older. Under 19. Pregnant. Caring for a child.
Does Medicare cover mental health?
Public insurance programs, such as Medicare and Medicaid, provide coverage. But some types of coverage may have limits or requirements. Plans offered through the Health Insurance Marketplace as part of the Affordable Care Act, or Obamacare, cover mental health and substance abuse, though the specific benefits depend on the state and the health plan.
Does Medicare cover inpatient rehab?
For example, Medicare only covers inpatient and outpatient rehab if the treatment is provided by a Medicare provider or facility, is deemed medically necessary, and a doctor establishes a treatment plan. 13 Medicaid coverage varies by state. Learn more about your state’s Medicaid coverage for substance abuse.
What is the ACA?
Often called “Obamacare,” the Affordable Care Act (ACA) works to insure more people with extended public and private coverage. 11,12. Specific to mental health and addiction, the ACA increases access in 3 ways: 11,12.
Can you have both Medicare and Medicaid?
Some people may qualify for both Medicare and Medicaid. These people with “dual-eligibility” will have very little out-of-pocket expenses. 8 Cost differences will vary by plan and state where coverage is received. Determine if you qualify for Medicaid here.
Can a health insurance plan deny coverage based on pre-existing conditions?
Health plans can no longer deny coverage based on pre-existing conditions or past history of addiction or substance dependence. Along with expanding coverage and offering parity, the ACA gives individuals access to the Health Insurance Marketplace.
How long does Medicare Part A cover?
This can either be in a regular hospital or psychiatric hospital. However, in cases of psychiatric hospitals, Part A only pays for 190 days of inpatient treatment per lifetime.
What is Medicare for people 65 and older?
In some cases, it also applies to those with end-stage renal disease. Medicare is divided into four parts: A (hospital insurance), B (medical insurance), C (Medicare Advantage) and D (prescription drugs). Inpatient Services.
What is the Mental Health Parity and Addiction Equity Act?
The Mental Health Parity and Addiction Equity Act of 2008 stipulates that insurance companies cannot discriminate against or deny coverage to individuals with substance use disorders. In addition, the Affordable Care Act of 2010 classified mental health and addiction services as essential health benefits.
When does Medicare start?
Testing or training for job skills. Medicare coverage begins on the first day of the month of the individual’s 65th birthday. Enrollment extends from three months prior to three months after the 65th birthday.
Who is Sonia Tagliareni?
Sonia Tagliareni is a writer and researcher for DrugRehab.com. She is passionate about helping people. She started her professional writing career in 2012 and has since written for the finance, engineering, lifestyle and entertainment industry. Sonia holds a bachelor’s degree from the Florida Institute of Technology.
What is parity protection?
Parity protection rules dictate that the financial, treatment and care management limits for mental and substance use disorders cannot be more than those placed on physical health treatment. The health marketplace insurance plan makes treatment for mental disorders and substance abuse more accessible.
Does Medicaid cover rehab?
Medicaid varies from state to state, and it offers coverage only to low-income individuals, families, children, pregnant women, the elderly and people with disabilities.
What does ACA cover?
The Affordable Care Act (ACA) lists drug or alcohol addiction services as 1 of 10 categories of essential health benefits, which means that any insurance sold on the Health Insurance Marketplace must cover treatment. 1 Insurance companies are required to cover certain basic health services, which include the treatment of mental and behavioral health conditions as well as substance use disorders (SUDs). Additionally, the Mental Health Parity and Addiction Equity Act (MHPAEA) ensures that all private insurance plans cover substance abuse treatment to the same degree that they cover other medical issues, so you can expect equal levels of coverage for both. 2
Does insurance cover substance abuse?
Additionally, the Mental Health Parity and Addiction Equity Act (MHPAEA) ensures that all private insurance plans cover substance abuse treatment to the same degree that they cover other medical issues, so you can expect equal levels of coverage for both. 2. Spanish Version. In addition, insurance companies cannot deny coverage for any pre-existing ...
How long does insurance cover outpatient care?
While some insurance companies offer policies that extend treatment coverage for up to six months or a year, others may stop coverage after days or weeks.
What is residential treatment?
Once a substance is fully eradicated from the patient’s body, they may choose to proceed to residential care. In residential care, a patient may participate in behavioral therapies effective for treating substance use disorders, such as: Cognitive behavioral therapy (CBT). Dialectical behavioral therapy (DBT).
What are the different types of residential care?
Once a substance is fully eradicated from the patient’s body, they may choose to proceed to residential care. In residential care, a patient may participate in behavioral therapies effective for treating substance use disorders, such as: 1 Cognitive behavioral therapy (CBT). 2 Dialectical behavioral therapy (DBT). 3 Group therapy.
What are the co-occurring mental health disorders?
Many people who struggle with addiction and substance abuse issues also struggle with a co-occurring mental health disorder, such as anxiety or depression. Treatment medications, therapy, and even time spent in residential drug rehab facilities on an inpatient basis are often covered. 4.
Does private insurance cover substance abuse?
Often, yes. Private insurance companies are now required by the Affordable Care Act (ACA) to provide some form of substance abuse treatment coverage to their members. The ACA also regards substance abuse treatment as an essential health care benefit for US citizens. This means most insurers can’t completely deny substance use disorder coverage.
What is medical necessity?
Medical necessity is when an insurance company determines that a physician would give the patient after exercising prudent clinical judgment. You can verify your insurance with AAC and learn more about addiction treatment plans and insurance coverage.
Does the ACA cover mental health?
In addition, the ACA also mandated that such policies cover the treatment of mental illness. Many people who struggle with addiction and substance abuse issues also struggle ...