
What do you need to know about acute inpatient rehabilitation?
Dec 20, 2018 · physician with specialized training and experience in inpatient rehabilitation. The requirement for medical supervision means that the rehabilitation physician must conduct face-to-face visits with the patient at least 3 days per week throughout the patient’s stay in the IRF to assess the patient both medically and functionally, as well as
What are the requirements for a rehabilitation center?
Sep 13, 2019 · Evaluation and counseling by psychiatrists, psychologists, and clinical nurse specialists to help the patient understand or change behaviors that cause the patient to refuse therapy may be more available at the IRF than a subacute unit.
What documentation is required for services in acute rehabilitation settings?
Nov 22, 2021 · MLN905643 - Inpatient Rehabilitation Therapy Services: Complying with Document Requirements Author: Centers for Medicare & Medicaid Services \(CMS\) Medicare Learning Network \(MLN\) Subject: Provider Compliance Keywords: MLN Created Date: 11/22/2021 4:06:10 PM
Who are the members of the rehabilitation center team?
Setting: United States inpatient rehabilitation facilities subscribing to the UDSMR. Participants: Patients 65 years or older (N=84.701) with primary diagnoses of debility (n=14,835), hip fracture (n=68,915), and myopathy (n=951). Interventions: Not applicable. Main outcome measures: Change in functional status, including efficiency (change in functional status divided by length …
What are some CMS criteria for inpatient rehabilitation facilities?
Rehabilitation Readiness Patient is willing and able to participate in a rehabilitation program. Patient must be able to participate in an intensive therapy program i.e., 3 hours per day, 5 to 6 days per week. Patients require two or more therapy disciplines. Patients require at least a five-day rehab stay.
What are the CMS 13 diagnosis?
Understanding qualifying conditions for admissionStroke.Spinal cord injury.Congenital deformity.Amputation.Major multiple trauma.Fracture of femur.Brain injury.Neurological disorders.More items...
What is IRF in healthcare?
IRFs are free standing rehabilitation hospitals and rehabilitation units in acute care hospitals. They provide an intensive rehabilitation program and patients who are admitted must be able to tolerate three hours of intense rehabilitation services per day.Dec 1, 2021
What is the IRF Pai?
The Inpatient Rehabilitation Facility Patient Assessment Instrument (IRF-PAI) is the assessment instrument IRF providers use to collect patient assessment data for quality measure calculation and payment determination in accordance with the IRF Quality Reporting Program (QRP).Apr 1, 2022
Which tool is administered to all patients admitted to an inpatient rehabilitation facility?
1 An Inpatient Rehabilitation Facility Patient Assessment Instrument (IRF PAI) is used to collect data that drives payment. It must be completed on admission and upon discharge of the patient from the IRF.
What is a rehab diagnosis?
The main difference is that in rehabilitation the presenting problems are limitations in activities and the main items investigated are impairment and contextual matters, whereas in medicine the presenting problems are symptoms, and the goals are the diagnosis and treatment of the underlying disease.
What is the difference between Ltac and rehab?
Staffing: Long-term acute care facilities typically employ a stable of in-house doctors, and patients will see a doctor at least once a day. Inpatient rehabilitation facilities and skilled nursing facilities also have physicians on staff, but therapists and nurses take on more of the daily care management.
What is the difference between Ltac and SNF?
Since LTACH residents typically stay for 30 to 60 days, as opposed to a SNF where stay is typically much longer, there is an increased possibility of swings in occupancy, revenue and staffing. Further, when an LTACH patient stays less than 25 days, the facility will not be approved for Medicare reimbursement.
What does ARU mean in healthcare?
Acute Rehabilitation UnitAcute Rehabilitation Unit (ARU)
What is a PPS coordinator?
The PPS coordinator is responsible for planning, developing and overall coordination of activities that support the Prospective Payment System (PPS) process for the inpatient rehabilitation unit.Jul 12, 2011
What is replacing FIM?
CARE stands for Continuity Assessment Record and Evaluation (CARE) Item Set. You can think of it as the replacement to FIM.May 18, 2021
What is the care tool?
The CARE tool is a set of data elements that was developed after Congress called on the Centers for Medicare and Medicaid Services, which you may know as CMS, to develop one comprehensive patient assessment instrument that could measure health and functional status across the post-acute care continuum.
What is the purpose of a post-admission physician evaluation?
The purpose of the post-admission physician evaluation is to document the patient’s status on admission to the IRF, compare it to that noted in the preadmission screening documentation, and begin development of the patient’s expected course of treatment that will be completed with input from all of the interdisciplinary team members in the overall plan of care. A dated, timed, and authenticated post-admission physician evaluation must be retained in the patient’s IRF medical record. The post-admission physician evaluation must:
What is an IRF in nursing?
Admission to an IRF is appropriate for patients with complex nursing, medical management, and rehabilitative needs.
What is CERT in Medicare?
This fact sheet describes common Comprehensive Error Rate Testing (CERT) Program errors related to inpatient rehabilitation services and provides information on the documentation needed to support a claim submitted to Medicare for inpatient rehabilitation services.
What is individualized overall plan of care?
The individualized overall plan of care is synthesized by the rehabilitation physician from the preadmission screening, post-admission physician evaluation, and information garnered from the assessments of all disciplines involved in treating the patient. The individualized overall plan of care must:
What is an IRF PAI?
The IRF-PAI gathers data to determine the payment for each Medicare Part A FFS patient admitted to an IRF. The IRF-PAI form must be included in the patient’s IRF medical record in either electronic or paper format.
Who generates admission orders?
Admission orders must be generated by a physician at the time of admission. Any licensed physician may generate the admission order. Physician extenders, working in collaboration with the physician, may also generate the admission order.
Patient Demographics
The following information comes from the National Outcomes Measurement System (NOMS) data collected by ASHA members across the country.
Reimbursement mechanism
Generally, a third party payer covers the cost of acute rehabilitation services, although coverage varies widely from policy to policy. Inpatient rehabilitation facilities (IRFs) are under a prospective payment system (PPS) which applies to patients who have Medicare as a primary payer.
Referral process
Individuals are referred for communication or swallowing evaluation by their attending physicians. In most settings, a physician's order is required for continued treatment.
Collaboration with other disciplines
Speech-language pathologists work in conjunction with the entire interdisciplinary rehabilitation team.
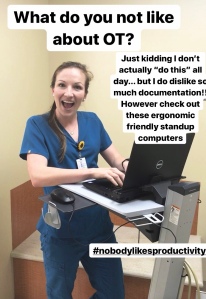
Documentation Requirements
Speech-language pathologists working in acute rehabilitation settings are required to document services in a medical record. Initial evaluations are conducted over a period of days, with subsequent progress documentation on at least a weekly basis.
What is inpatient rehab coding?
Inpatient rehab coding involves reading proper, clear documentation, as well as skillful, accurate, and detailed abstraction of the POA diagnosis code, sequela effects, ongoing comorbidities, forever diagnosis codes, chronic conditions, use of assistive devices, and complications.
What is ADL in healthcare?
While providing quality care, skilled clinicians must assess the patient’s activities of daily living (ADL) functions in the presence of illness. They must also justify the patient’s etiology for complications and comorbidities in the medical record.
Who is Tamara Thivierge?
Tamara Thivierge, MHA, CPC, is a certified medical coder with over 25 years of broad professional history in diverse settings, including inpatient rehab, behavioral health center, family physicians, and auditing with an insurance payer. She has also led workshops on billing in the Hampton Roads, Va., area.
.jpg?width=600&name=Americus Rehab Therpay (9668).jpg)
Patient Demographics
Reimbursement Mechanism
Referral Process
- Individuals are referred for communication or swallowing evaluation by their attending physicians. In most settings, a physician's order is required for continued treatment.
Collaboration with Other Disciplines
- Speech-language pathologists work in conjunction with the entire interdisciplinary rehabilitation team. This team consists of the patient, family, physicians, nurses, physical therapists, occupational therapists, psychologists, dietitians, recreation therapists, music therapists, vocational rehabilitation counselors, and social workers/case managers. Rehabilitation professi…
Documentation Requirements
- Speech-language pathologists working in acute rehabilitation settings are required to document services in a medical record. Initial evaluations are conducted over a period of days, with subsequent progress documentation on at least a weekly basis. A discharge summary assists with continued care/continuity of patient care as the patient transitions...
Resources
- Go to the SLP Health Caresection of ASHA's Web site to access: 1. ASHA Speech-Language Pathology Health Care Survey 2. Health care frequently asked questions (FAQs) 3. ASHA member forums 4. Issue Briefs Go to the Billing and Reimbursementsection of the ASHA website to access: 1. Medicare Fee Schedule 2. Billing and coding information 3. Reimbursement frequentl…