The short answer: It depends on how long you're receiving care. The longer answer: Medicare will cover 100% of the first 20 days of rehabilitation in a long-term care facility, as long as you continue to meet criteria (see below) to qualify for coverage during those 20 days. 4 Beginning on day 21, you will be responsible for a co-payment per day.
Full Answer
Does Medicaid pay for long-term care?
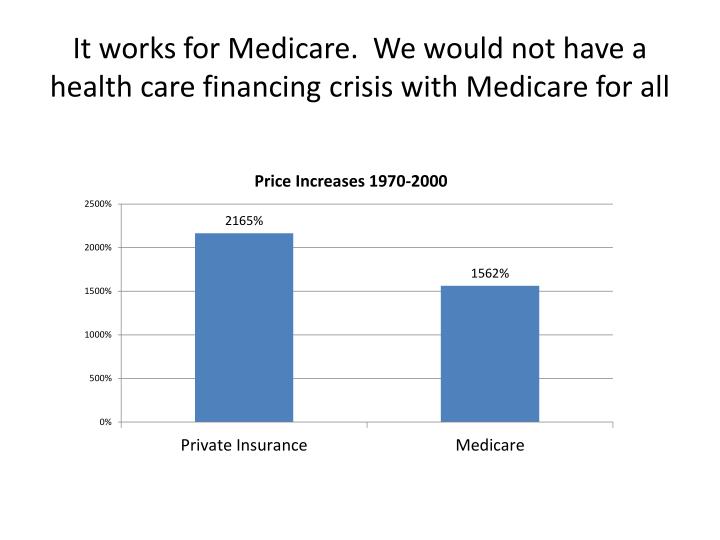
Dec 14, 2021 · This is because private pay residents pay approximately 25% more for nursing home care than Medicaid pays. In 2022, the nationwide average private payer pays approximately $255 / day for nursing home care while Medicaid pays approximately $206 / day. Search for Medicaid nursing homes here. Being Medicaid eligible and finding a Medicaid nursing ...
Why do States pay for long term care instead of nursing home?
Nursing Facility Services are provided by Medicaid certified nursing homes, which primarily provide three types of services: Skilled nursing or medical care and related services; Rehabilitation needed due to injury, disability, or illness; Long term care —health-related care and services (above the level of room and board) not available in the community, needed regularly …
Why does private pay pay more for nursing home care than Medicaid?
Feb 28, 2022 · Over the years, Medicaid’s coverage of long term care has expanded to include long term services and supports (LTSS) via Home and Community Based Services (HCBS) Medicaid Waivers, also called 1915(c) waivers. This is because it is more cost efficient for the state to pay for long term care that prevents and / or delays the need for institutionalization …
How much does Medicaid pay for a nursing home a day?
Jan 31, 2022 · Medicaid was the source of payment for more than 42% of all births in the U.S. in 2018. 7 In 2017, Medicaid paid for more than 30% of long-term care for those in nursing care facilities and continuing care retirement communities. 7 Facilities that specialize in …

What is NF Medicaid?
A NF participating in Medicaid must provide, or arrange for, nursing or related services and specialized rehabilitative services to attain or maintain the highest practicable physical, mental, and psychosocial well-being of each resident.
What is long term care?
Long term care —health-related care and services (above the level of room and board) not available in the community, needed regularly due to a mental or physical condition. A nursing facility is one of many settings for long-term care, including or other services and supports outside of an institution, provided by Medicaid or other state agencies.
What are the requirements for nursing home?
Federal requirements specify that each NF must provide, (and residents may not be charged for), at least: 1 Nursing and related services 2 Specialized rehabilitative services (treatment and services required by residents with mental illness or intellectual disability, not provided or arranged for by the state) 3 Medically-related social services 4 Pharmaceutical services (with assurance of accurate acquiring, receiving, dispensing, and administering of drugs and biologicals) 5 Dietary services individualized to the needs of each resident 6 Professionally directed program of activities to meet the interests and needs for well being of each resident 7 Emergency dental services (and routine dental services to the extent covered under the state plan) 8 Room and bed maintenance services 9 Routine personal hygiene items and services
What is the definition of NF in Medicaid?
Specific to each state, the general or usual responsibilities of the NF are shaped by the definition of NF service in the state's Medicaid state plan, which may also specify certain types of limitations to each service. States may also devise levels of service or payment methodologies by acuity or specialization of the nursing facilities.
Where are the requirements for Medicaid nursing facilities?
Specific requirements for Medicaid nursing facilities may be found primarily in law at section 1919 of the Social Security Act , in regulation primarily at 42 CFR 483 subpart B, and in formal Centers for Medicare & Medicaid Services guidance documents. Also see:
What services does a NF need?
Federal requirements specify that each NF must provide, (and residents may not be charged for), at least: Nursing and related services. Specialized rehabilitative services (treatment and services required by residents with mental illness or intellectual disability, not provided or arranged for by the state) Medically-related social services.
What is medically related social services?
Medically-related social services. Pharmaceutical services (with assurance of accurate acquiring, receiving, dispensing, and administering of drugs and biologicals) Dietary services individualized to the needs of each resident.
What is community spouse resource allowance?
That said, there is a community spouse resource allowance, which allows a greater portion of the couple’s assets to be allocated to the non-applicant spouse without impacting the applicant spouse’s long term care Medicaid eligibility.
What is HCBS Medicaid?
Over the years, Medicaid’s coverage of long term care has expanded to include long term services and supports (LTSS) via Home and Community Based Services (HCBS) Medicaid Waivers, also called 1915 (c) waivers. This is because it is more cost efficient for the state to pay for long term care that prevents and / or delays ...
How much is the home equity interest for Medicaid in 2021?
As of 2021, this amount is generally $603,000 or $906,000, depending on the state.
How old do you have to be to qualify for Medicaid?
• Be a resident of the state in which one is applying for Medicaid benefits. • Be 65 years of age or older, permanently disabled, or blind. • Have monthly income and countable assets under a specific level.
How long does Medicaid look back?
In the majority of the states, the “look back” is for 60-months.
What is Medicaid for seniors?
Medicaid, which is a needs-based healthcare program for persons of all ages, covers the cost of long term care for seniors and disabled individuals who meet their state’s eligibility requirements. There are several Medicaid programs from which one can receive this type of care.
What is the state plan option 1915?
Via this option, a state can target a specific population and only this group of people can receive home and community based services.
How many people will be on medicaid in 2020?
Medicaid combined with the Children’s Health Insurance Program serves more than 72.5 million people in the U.S. 2. As of 2020, the average monthly number of people served through Medicaid was estimated to be 15.9 million adults and 28.9 million children. 15.
What is detox program?
Detox is the first stage of addiction treatment and helps you safely withdraw from drugs and alcohol in a controlled, supervised medical setting.
How many hours of rehab do you get with medicaid?
Most rehabs that take Medicaid generally provide programs provide medical care and substance rehabilitation —including group and individual therapy, 12-step meetings, and other recovery activities—24 hours per day in a highly structured setting.
How is naltrexone used?
Naltrexone is used to decrease the risk of relapse by blocking the effects of other opioids; naltrexone may be administered after successful withdrawal management and detox completion. 13. These treatment medications are often combined with behavioral therapies.
What is behavioral therapy?
Behavioral counseling and therapy are used to engage patients in their addiction treatment and help them reframe thoughts, attitudes, and behaviors surrounding substance abuse. Cognitive behavioral therapy, contingency management, community reinforcement, and motivational enhancement are just some of the therapies and counseling approaches used in substance abuse treatment. 12
What is a dual eligible beneficiary?
Someone who has both types of coverage is known as a dual-eligible beneficiary. 16 Medicare typically pays for Medicare covered services first and then Medicaid tends to cover services Medicare does not cover. In 2018, 12.2 million individuals were simultaneously enrolled in both Medicaid and Medicare. 17.
How many people are covered by medicaid?
Medicaid is a state and federal health insurance program that, combined with the Children’s Health Insurance Program, serves more than 72.5 million people in the U.S. 2 Low-income families, disabled adult children, and qualified pregnant women are just some groups that all states are required to cover through Medicaid.
What are the programs of the ADA?
The programs and partnerships contained in this section are aimed at achieving a system that is: 1 Person-driven: The system affords older people, people with disabilities and/or chronic illness the opportunity to decide where and with whom they live, to have control over the services they receive and who provides the services, to work and earn money, and to include friends and supports to help them participate in community life. 2 Inclusive: The system encourages and supports people to live where they want to live with access to a full array of quality services and supports in the community. 3 Effective and accountable: The system offers high quality services that improve quality of life. Accountability and responsibility is shared between public and private partners and includes personal accountability and planning for long-term care needs, including greater use and awareness of private sources of funding. 4 Sustainable and efficient: The system achieves economy and efficiency by coordinating and managing a package of services paid that are appropriate for the beneficiary and paid for by the appropriate party. 5 Coordinated and transparent: The system coordinates services from various funding streams to provide a coordinated, seamless package of supports, and makes effective use of health information technology to provide transparent information to consumers, providers and payers. 6 Culturally competent: The system provides accessible information and services that take into account people's cultural and linguistic needs.
Why do people need long term care?
Millions of Americans, including children, adults, and seniors, need long-term care services because of disabling conditions and chronic illnesses. Medicaid is the primary payer across the nation for long-term care services.
What is Medicaid LTSS?
Medicaid allows for the coverage of these services through several vehicles and over a continuum of settings, ranging from institutional care to community-based long-term services and supports (LTSS).
What is accountability and responsibility?
Accountability and responsibility is shared between public and private partners and includes personal accountability and planning for long-term care needs, including greater use and awareness of private sources of funding.
What is Medicaid for low income?
Medicaid pays for health care services for those individuals with low income and assets who may incur very high medical bills.
What is a Medicaid certified nursing home?
Medicaid certified nursing homes deliver specific medically indicated care , known as Nursing Facility Services , including: Medicaid coverage for Nursing Facility Services only applies to services provided in a nursing home licensed and certified as a Medicaid Nursing Facility (NF).
How long does a person live with hospice?
You have elected to no longer seek a cure. Your life expectancy is six months or less. Hospice care may be received in your home, in a nursing home, or a hospice care facility. Short-term hospital stays and inpatient care may also be approved for Medicare payment (for caregiver respite).
How long can you stay in an SNF?
If your stay in an SNF exceeds 100 days, or your ability to pay co-pays ends before the 100th day is reached, you may no longer be eligible to stay in the Medicare-certified SNF under Medicare coverage.
What does the VA pay for?
The VA may also pay for long-term care services required by veterans who do not have service-related disabilities but are incapable of paying for essential care. In these cases, services may require a sliding scale co-pay based on patient income level.
Can you recover Medicaid for nursing home?
If you received Medicaid coverage for long-term care services, the state can choose to recoup Medicaid costs. Federal law provides states with the ability to recover any or all costs incurred by Medicaid for long-term care services, including nursing home, home, or community-based services.
Does Medicare pay for physical therapy?
Provided you meet the above conditions, Medicare will pay a portion of the costs during each benefit period for a limited number of days.
Can you sell your home to pay for long term care?
Depending on the situation, you can in fact be forced to sell your home to help pay for long-term care . This can occur once you have spent down your assets and successfully applied for Medicaid.
Is rehab a long term care?
For many, rehabilitation after an injury or illness serves as their first introduction to long-term care . Although these rehab stints are often short-term in nature, the admission process is similar to the application process for permanent placement in a nursing home. In both cases, disclosure of financial and insurance coverage information is needed to determine placement.
What is Intensive Outpatient Services?
Intensive outpatient services, otherwise known as partial hospitalization. Inpatient or residential services. Early intervention. The treatment that are covered by drug and alcohol rehabilitation programs that accept Medicaid might also include the prescription drugs that are provided through MAT (medication assisted treatments).
What drugs are used for opioid addiction?
If you have an opioid use disorder, therefore, these drugs may include buprenorphine (both naloxone and buprenorphine), naltrexone, and methadone. On the other hand, if you are addicted to alcohol, the medications may include naltrexone, disulfiram, and acomprosate. Overall, alcohol and drug treatment centers that accept Medicaid are crucial ...
Why are alcohol and drug treatment centers important?
Overall, alcohol and drug treatment centers that accept Medicaid are crucial because they have made it possible for more individuals struggling with addiction offset the cost of their rehabilitation.
How many people are on medicaid in 2017?
Medicaid is so widespread that by 2017 more than 68 million Americans were enrolled into the program. For these individuals - as well as their families - the key to using the benefits offered lies in recognizing how coverage works for the treatment of drug and alcohol addiction and substance use disorders.
How is the drug rehab program funded?
As such, this program is funded through partnerships between the federal government and states. However, you should consider that the exact nature of your insurance coverage for drug rehabilitation programs that accept Medicaid will vary ...
Do you have to apply for medicaid before getting a caseworker?
Even in cases where you may not be sure about your qualification status, it is vital that you apply for Medicaid before getting qualified caseworkers to evaluate your specific situation. This may be the only choice you have to offset the cost of the alcohol and drug rehab you require.
What are resources and income?
Your resources and income (if any), including items you can sell for cash, real property, and bank accounts. Whether you are a legal immigrant or an US citizen. That said, the rules that apply to counting your resources and income will vary from one state to another in addition to from one group to another.
How often is a care plan made?
A full care plan is made once a year with updates every 3 months. Residents and their family members are always invited to these meetings. Ask when they will happen. If you cannot attend, ask if it can be held at another time or if you can join in by phone.
What do staff members do when family members move to long term care?
This is a big change in your role. Staff members now help your family member with medication, treatment, bathing, dressing, eating, and other daily tasks.
How long does it take for a family member to go to rehab?
Your family member’s progress in rehab is discussed at a “care planning meeting.” This takes place about 3 weeks after admission to rehab. At this meeting, staff members talk about your family member’s initial treatment goals and what he or she needs for ongoing treatment and follow-up care. It may be clear by this meeting that your family member cannot go home safely.
What to look for when family member does not speak English?
If your family member does not speak English, then look for residents and staff who can communicate in his or her language.
When should family planning start?
Planning should start as soon as you know that your family member is going to a long-term setting. This can be a very hard transition for patients and family members.
Do I need to apply for medicaid for nursing home?
may need to apply for Medicaid. This is because Medicare and most private insurance do not pay for long-term nursing home care. You can ask the social worker on the rehab unit to help you with the paper work. This process can take many weeks.
How much does Medicaid cost for skilled nursing?
Medicaid Benefits provides Savings for You! • Skilled Nursing Care and Rehabilitation or “Nursing Homes” Costs around $11,000/month. Medicaid Beneficiaries maximum payment or patient responsibility to the skilled nursing facility is their income less $130, which they are able to keep for their own personal needs.
Does Florida have Medicaid?
Medicaid is a state funded program that provides financial coverage for Long Term Custodial Care. It is different from Medicare, as Medicare does not pay for Long Term Care. Medicare and Medicaid work together to cover the medical expenses of an individual for as long as those services are deemed necessary.