
How long does it take to recover from postpartum depression?
May 03, 2019 · Due to the personal nature of postpartum depression, there is no definite recovery timeline. While most cases heal within one year after symptoms begin, many women might still experience postpartum depression symptoms years after their onset.
When to stop treatment for postpartum depression?
Depending on the severity of the depression, treatment may last a few weeks to a few months or longer. Counseling for postpartum depression will allow an individual to talk about their problems, their depression and to set realistic goals for solving the problem and for coping with the disorder.
When does postpartum depression start after childbirth?
Apr 09, 2022 · Electroconvulsive Therapy for Postpartum Depression. For individuals experiencing severe PPD, particularly those with psychotic symptoms related to their disorder, some providers have recommended Electroconvulsive Therapy (ECT). Research has shown that this can help alleviate psychotic and depressive symptoms of PPD, especially in the early ...
When to see a doctor for postpartum depression?
According to the DSM-5, a manual used to diagnose mental disorders, PPD is a form of major depression that begins within 4 weeks of giving birth. Therefore, Our urgentway healthcare providers give the open Umbrella of postpartum depression Treatment.
What is the treatment for postpartum depression?
Postpartum depression. Postpartum depression is often treated with psychotherapy (also called talk therapy or mental health counseling), medication or both. Psychotherapy. It may help to talk through your concerns with a psychiatrist, psychologist or other mental health professional.
How to treat postpartum psychosis?
Treatment may include: Medication. Treatment may require a combination of medications — such as antipsychotic medications, mood stabilizers and benzodiazepines — to control your signs and symptoms.
What is ECT therapy?
ECT is a procedure in which small electrical currents are passed through the brain, intentionally triggering a brief seizure. ECT seems to cause changes in brain chemistry ...
Can postpartum depression be chronic?
With appropriate treatment, postpartum depression symptoms usually improve. In some cases, postpartum depression can continue, becoming chronic depression. It's important to continue treatment after you begin to feel better. Stopping treatment too early may lead to a relapse.
Does ECT cause depression?
ECT seems to cause changes in brain chemistry that can reduce the symptoms of psychosis and depression, especially when other treatments have been unsuccessful. Treatment for postpartum psychosis can challenge a mother's ability to breast-feed.
Is postpartum depression a medical condition?
But remember, postpartum depression is never anyone's fault. It's a common medical condition that needs treatment. So, if you're having trouble coping with postpartum depression, talk with a therapist. Ask your doctor or therapist about local support groups for new moms or women who have postpartum depression.
What to do if your thyroid is underactive?
Order blood tests to determine whether an underactive thyroid is contributing to your signs and symptoms. Order other tests, if warranted, to rule out other causes for your symptoms.
What are the symptoms of a postpartum depression episode?
However, studies suggest that depressive episodes are significantly more common in women in the first three months after delivery, 32 and an increased vulnerability to psychiatric illness may persist for a year or more. 33 It is important to differentiate PPD from other psychiatric and nonpsychiatric diagnoses. The “postpartum blues” or “baby blues” is a transient mood disturbance that affects up to 75% of new mothers in the 10 days following delivery, and consists of crying, irritability, fatigue, anxiety, and emotional lability. Symptoms are generally mild and self-limited, and do not involve total loss of pleasure or interest, persistent low mood, or suicidal ideation. 34 On the other extreme, postpartum psychosis is a psychiatric emergency that requires immediate intervention, and is characterized by the rapid onset of severe mood swings, a waxing and waning sensorium, delusions, hallucinations or disorganized behaviors, and a relatively high incidence of suicidal ideation or homicidal ideation toward the infant. 35 Women presenting with a depressive episode, mood elevation, or psychotic symptoms should be screened for any prior history of mania or hypomania to rule out previously undiagnosed bipolar disorder. 36 Anxiety disorders are common in perinatal women, and women may have depression comorbid with obsessive-compulsive symptoms, generalized anxiety disorder, panic disorder or post-traumatic stress disorder. 37 Substance use and medical causes of psychiatric symptoms, such as thyroid disorders, should also be considered.
What is the best treatment for perinatal depression?
Massage as treatment for perinatal depression has also been examined independently, and modalities include therapeutic massage, partner-delivered massage, and instruction in infant-massage in the postpartum period.
How long can a woman breastfeed?
The benefits of breastfeeding have been well described 66 – 73 and have led the World Health Organization, the American Academy of Pediatrics and the American Academy of Family Practitioners to recommend breastfeeding for at least the first 6 months for most women. 66, 67, 73 Potential effects of antidepressant medication on breastfeeding are of concern to many mothers and clinicians. 49, 74 Neonates and young infants are especially vulnerable to potential drug effects due to their immature hepatic and renal systems, immature blood–brain barriers, and developing neurological systems. 75, 76 Because relatively little is known about the effects of antidepressant medication in breast milk, some experts have recommended nonpharmacologic treatment modalities when possible, particularly for mild to moderate depression. 76 However, non-pharmacologic treatments are not effective for some women, and may not be accessible for many women.
What is interpersonal therapy?
Interpersonal therapy (IPT) is a time-limited treatment for major depression based on addressing the connection between interpersonal problems and mood, 98 which frames depression as a medical illness occurring in a social context. 99 In IPT, the patient and clinician select one of four interpersonal problem areas (role transition, role dispute, grief, or interpersonal deficits) as a treatment focus. Over the course of the therapy (typically 12–20 weeks), strategies are pursued to assist patients in modifying problematic approaches to relationships and in building better social supports. IPT has been adapted to address problem areas relevant to postpartum depression such as the relationship between mother and infant, mother and partner, and transition back to work. 100 The fact that IPT is both time-limited and problem-focused fits well with the demands of the postpartum mother.
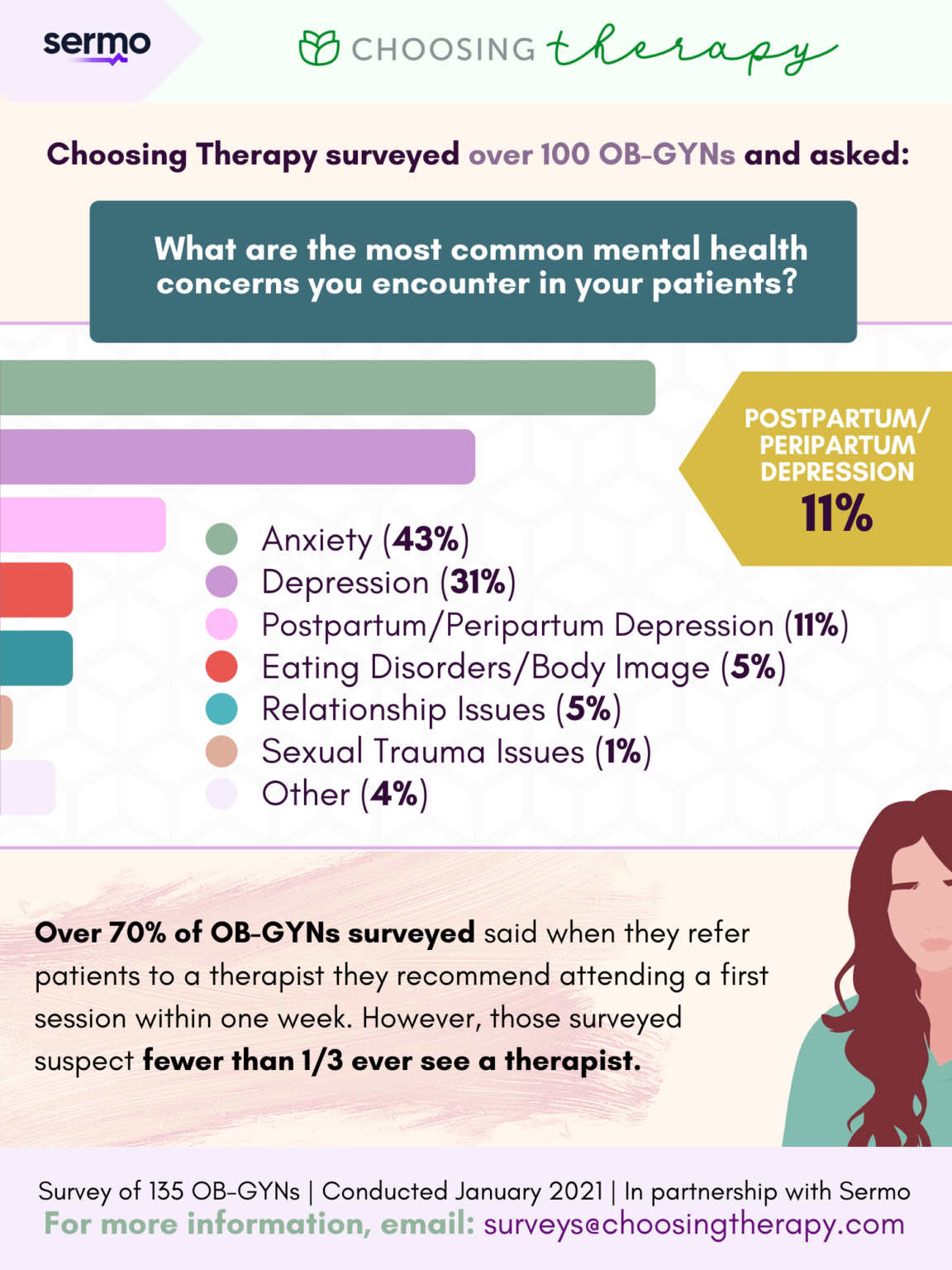
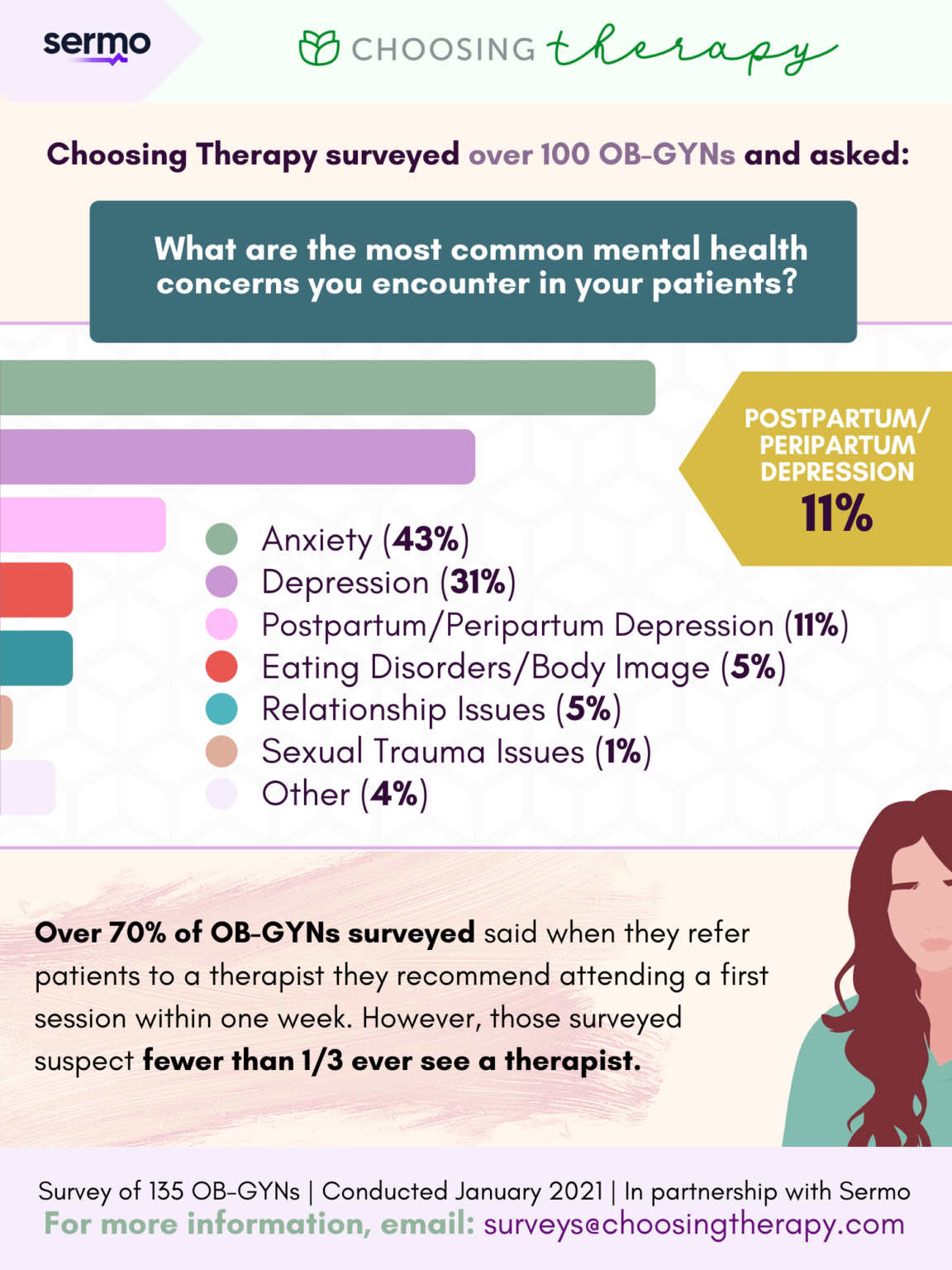
How many mothers are affected by postpartum depression?
Postpartum depression is a major international public health problem that affects at least 1 in 8 mothers and their children in the year after childbirth worldwide. PPD may be more common and may be associated with more morbidity for both mothers and children in resource-poor countries.
Is postpartum depression a major depression?
A small but growing literature suggests that postpartum depression can be thought of as a variant of major depression that responds similarly to antidepressant medication. 46, 47 Concerns unique to pharmacologic treatment of PPD include metabolic changes in the postpartum period, exposure of the infant to medication in breast milk, the effect of depression and treatment on the ability of the depressed mother to care for a new baby, and the perceived stigma of being seen as a “bad mother” for requiring medication. 48 – 50 These factors, as well as the woman’s level of distress, access to care, and experience with past treatment may influence the decision of the patient and her caregiver regarding the choice of pharmacologic and nonpharmacologic treatments for PPD. Data comparing the effectiveness of medication against other treatment modalities for PPD are scarce, though do suggest that medications are at least as effective as most psychological interventions based on effect size. 51 To date, four randomized controlled studies on the treatment of PPD with antidepressant medications have been published, along with several open trials. Additionally, two randomized studies have looked at the prevention of PPD with antidepressant medication.
What is psychosocial intervention?
As compared with IPT or CBT, psychosocial interventions are unstructured and nonmanualized, and include nondirective counseling and peer support. Nondirective counseling (also known as “person-centered”) is based on the use of empathic and nonjudgmental listening and support. In the first notable study evaluating this intervention, Holden randomized 50 women with PPD to 8 weekly nondirective counseling sessions with a health visitor or routine primary care. 108 A health visitor in the UK is a public health nurse who conducts home visits with pregnant and postpartum women. This study found that the rate of recovery from PPD for counseling (69%) was significantly greater than that of the control group (38%). In a similar study conducted in Sweden, Wickberg and Hwang randomized 31 women with PPD to receive six nondirective counseling sessions by child health clinic nurses or routine primary care. 109 As in the Holden study, a significantly greater percentage of women in the treatment group (80%) had remission of depression than in the control group (25%). Study limitations include the removal of four study participants, two in each group, for more intensive mental health services due to illness severity.
Diagnosis
Treatment
Clinical Trials
Lifestyle and Home Remedies
Coping and Support
- Your doctor will usually talk with you about your feelings, thoughts and mental health to distinguish between a short-term case of postpartum baby blues and a more severe form of depression. Don't be embarrassed ― postpartum depression is common. Share your symptoms with your doctor so that a useful treatment plan can be created for you. As part of your evaluatio…
Preparing For Your Appointment
- Treatment and recovery time vary, depending on the severity of your depression and your individual needs. If you have an underactive thyroid or an underlying illness, your doctor may treat those conditions or refer you to the appropriate specialist. Your doctor may also refer you to a mental health professional.