Medicare and Medicaid plans under Aetna provide coverage for outpatient drug and alcohol rehab if deemed necessary by a provider. The addiction treatment that Medicare covers may include intensive outpatient programs, which meet a few hours a week, and partial hospitalization programs, which meet 20 hours a week or more. 10
Full Answer
Is Aetna and Medicaid the same?
Aetna and Medicaid. We manage plans across the country including the Children's Health Insurance Plan (CHIP), plans for people on Medicaid and Medicare and long-term care programs. Our plans go by different names in different states, but they all offer the same high-quality care. Loading, please wait. state.
What is Aetna better health?
Mar 01, 2022 · The type of addiction treatment needed depends on several factors, such as the specific kind of substance being used, scope of addiction, and so on. Aetna’s in-network insurance plans cover a wide range of treatments for drug and alcohol use disorders in Florida, including: 4. Medically assisted detox —This type of treatment program assists ...
Why Aetna Medicaid administrators LLC?
Aetna Better Health offers Medicaid plans in many states across the country. Learn more about what Medicaid health plans are available to you. ... Understanding Medicaid can be tough. We have the resources and expertise to answer all your questions. And we’ll help you and your family get the care you need. ... Or choose “Go on” to move ...
Do you qualify for Medicaid?
Dec 07, 2021 · American Addiction Centers (AAC) is a leading provider of drug and alcohol addiction treatment and is in network with many of the top insurance providers in the U.S. Call to speak with an admissions navigator at (888) 319-2606. Helpline Information.
Choose your plan
Error or missing data. Please check your entries for an error message.
COVID-19
Get answers to your questions about COVID-19 testing and vaccines. You can protect yourself, your community and the “doers” who’ve helped protect us all.
Have questions about Medicaid?
Understanding Medicaid can be tough. We have the resources and expertise to answer all your questions. And we’ll help you and your family get the care you need. Check out our "Do I qualify for Medicaid?" article to learn more about Medicaid.
National experience, local impact
Aetna Better Health is proud to be part of the CVS Health ® family. Together, we share a vision to be a trusted health partner in the local communities we serve. We go beyond offering a traditional medical approach by providing a full array of services that enhance overall wellness and improve everyday life.
Do you have any questions about a specific health plan?
Visit the "Contact us" page to connect with Member Services in your state.
What is outpatient treatment?
Outpatient treatment allows you to receive help for your substance addiction without living in a center or program facility. You’ll need to choose a program that’s approved and covered by Aetna insurance. The insurance company will want to verify that the plan is effective and uses evidence-based treatment.
Is addiction treatment important?
Addiction treatment is a significant and important step, and the good news is that it’s more accessible today than it has been in the past. To find out the specifics, including copays and deductibles, it’s important to contact the insurer directly. Treatment is the first step on a journey to a long and happy life.
Does Aetna cover rehab?
Are rehabs covered by Aetna? Different Aetna medical insurance policies will have different levels of healthcare coverage for substance abuse treatment. While basic addiction treatment coverage is required by the Affordable Care Act, the exact programs covered and the deductibles or copayments that apply will vary based on your policy. 1 Aetna has a program called Screening, Brief Intervention and Referral to Treatment (SBIRT) that is used to help treat addiction and reduce the severity of use and trauma that results. 2 To participate, a patient has to have an Aetna Insurance health plan and be at least 9 years old.
Does Aetna have Medicare?
If you have Medicare through Aetna, your coverage will be different than a traditional health plan. Aetna Medicare Advantage works alongside your traditional Medicare coverage. 3 It helps you access expanded treatment options and may offer lower deductibles and copayments.
Does Aetna cover inpatient treatment?
However, the exact amount of coverage you have may vary, so be sure to fully understand the details of your insurance plan. Not all inpatient treatment programs will be covered.
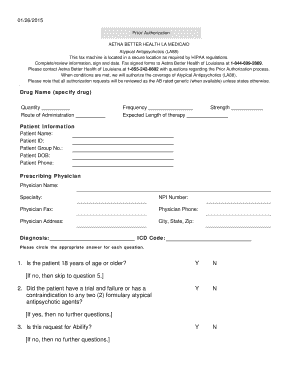
Does Aetna require preauthorization?
Aetna insurance for outpatient treatment may require preauthorization before you enroll. Work closely with the insurer so that they are aware of the program you’re choosing and when you’re scheduled to begin.
Does Aetna cover addiction?
An Aetna medical coverage policy should provide at least some coverage for addiction treatment. However, the exact programs covered and how much of the payment you’re responsible for will vary. You’ll want to contact the insurance provider to determine what your financial responsibility will be as you seek treatment.
What is deductible insurance?
A deductible is a fee you are responsible for before the insurer contributes to the cost of treatment. You also must pay 20% of the costs of inpatient treatment. 6 Aetna offers numerous plans that provide Medicare coverage. 2.
Does Medicare cover alcohol rehab?
Medicare and Medicaid plans under Aetna provide coverage for outpatient drug and alcohol rehab if deemed necessary by a provider. The addiction treatment that Medicare covers may include intensive outpatient programs, which meet a few hours a week, and partial hospitalization programs, which meet 20 hours a week or more. 10.
Does Aetna offer Medicaid?
Aetna Medicaid is offered in several states including California, Illinois, New York, and Florida. 3
Does Aetna cover inpatient rehab?
Some Aetna plans also cover inpatient rehab. For example, one Aetna plan in Maine for government employees has a $400 individual deductible and an $800 family deductible. After meeting your deductible, this Aetna plan covers the costs of inpatient treatment except for a 10% co-insurance payment.
Is Aetna a CVS?
Aetna is a part of the CVS Health Corporation 1 and provides a wide variety of insurance products to individuals and employers who provide group coverage to their employees. Aetna also offers plans for managed Medicare and managed Medicaid plans in 14 states. 2,3.
Does Aetna have HMO?
Aetna has a handful of HMO plans that help cover various recovery steps, ensuring that you get the best care possible within your HMO coverage area, each of which is designed to handle many payment situations.
Does Aetna cover addiction?
If you work within a PPO coverage area, your Aetna policy may cover your addiction treatment. These types of networks are often based on your recovery needs, so make sure to talk to your provider first.
What Addiction Treatment Services Are Covered By Medicaid In Kentucky?
Kentucky Medicaid provides beneficiaries with many behavioral health and substance use disorder treatment services so that everyone can get the treatment they need.
Top 5 Rehab Centers In Kentucky That Accept Medicaid
Out of all the drug rehab centers that take Kentucky Medicaid, we’ve chosen five for this list.
Factors That Affect Kentucky Medicaid Coverage For Addiction Treatment
Some factors might affect your overall cost for addiction treatment. The items described below will help to determine your out-of-pocket costs.
Who Qualifies For Kentucky Medicaid?
Individuals applying for Kentucky Medicaid must be low-income residents of the state. For a single person, the income limit is $217 and the resource limit is $2,000.
How To Use Your Kentucky Medicaid Plan For Drug Rehab
To use your Kentucky Medicaid plan for substance abuse treatment, you need to enroll in a health plan.
Kentucky Medicaid Insurance Coverage For Drug And Alcohol Rehab FAQs
Here we’ve answered some of the most commonly asked questions about Medicaid coverage for drug and alcohol addiction treatment in Kentucky.
Call Us To Find Drug Or Alcohol Rehab In Kentucky
Rehab programs can get very pricey, but with the help of Kentucky Medicaid affordable care is possible.
Does Aetna Cover Rehab for Drugs and Alcohol?
Aetna is a nationwide insurance provider offering plans that coverage for detox, rehab, and other forms of addiction treatment. The Affordable Care Act that was passed in 2010 requires most insurance plans to include alcohol and drug rehab coverage as an essential benefit. 7
How to Use Your Aetna Coverage for Rehab
To enter a specific addiction treatment program, you may need a referral from your primary doctor. They may give you some medication to help with withdrawal symptoms before you enter the drug rehab program. Once you are in the rehab process, you’ll have a monitored detox to ensure that the drugs leave your system safely.
How to Check Your Aetna Plan Details
To know for sure whether or not your Aetna insurance plan covers substance abuse rehab, it’s important to verify your coverage. You can use access details about your Aetna rehab coverage by logging on to Aetna’s member care website.
Types of Aetna Plans Covering Rehab Services
Aetna provides healthcare coverage for 39 million people in the United States. Aetna offers a variety of health insurance plans, Medicaid and Medicare coverage, and behavioral and medical management programs. 1, 2
How to Find Rehabs that Accept Aetna Coverage
If you are looking for rehab centers covered by Aetna, you can always call Aetna to verify coverage or by calling the American Addiction Centers detox helpline. Our rehab admissions team can review your plan and help you connect with rehabs that our centers accepting aetna.
How to check if Aetna covers rehab?
If you want to confirm if Aetna covers drug rehab or just check your insurance coverage, you can do so by calling the number on the back of your insurance card and speaking with a representative. You can also view your coverage by using an online account.
What is Aetna insurance?
Aetna Insurance was started in 1853 and has grown over the years. 1 It is now a part of CVS Health Corporation and provides health insurance to nearly 40 million people. 1, 2 Aetna plans cover medical, dental, behavioral health, and pharmacy care. 2. American Addiction Centers (AAC) is a leading provider of drug and alcohol addiction treatment ...
How much does Aetna pay?
Aetna pays about 80% of the cost of care after the deductible is met. Gold plans—These cost the most in premiums but have the lowest deductibles and will cost you the least in out-of-pocket expenses. Aetna pays about 90% of the cost of care after the deductible is met.
Does Aetna cover mental health?
You may have concerns about Aetna insurance mental health coverage, but under the Affordable Care Act, this is covered as an essential health benefit. 8 Depending on your insurance plan, Aetna drug and alcohol rehab coverage may include: Detoxification. Inpatient treatment. Partial hospitalization programs.
Does Aetna cover addiction?
Aetna insurance therapy coverage can be confusing to navigate, but a wide range of plans are available. Benefits do cover treatment for addiction, although what is covered and where you can seek treatment may depend on what type of plan you have. It is always a good idea to confirm your coverage before starting treatment.
What is intensive outpatient treatment?
Intensive outpatient treatment. Outpatient treatment. Services are often based on medical necessity and may require a referral and prior authorization to be approved. If you aren’t sure if your insurance will be accepted at American Addiction Centers (AAC), you can check on this page.
Does HMO cover PPO?
HMO plans cover only in-network providers, and that may be limited by geographic area, while PPO plans may provide more coverage for providers outside of your state. However, checking with your plan to ensure that you will be covered first is always a good idea.
