
What forms do you bill for drug and alcohol rehab?
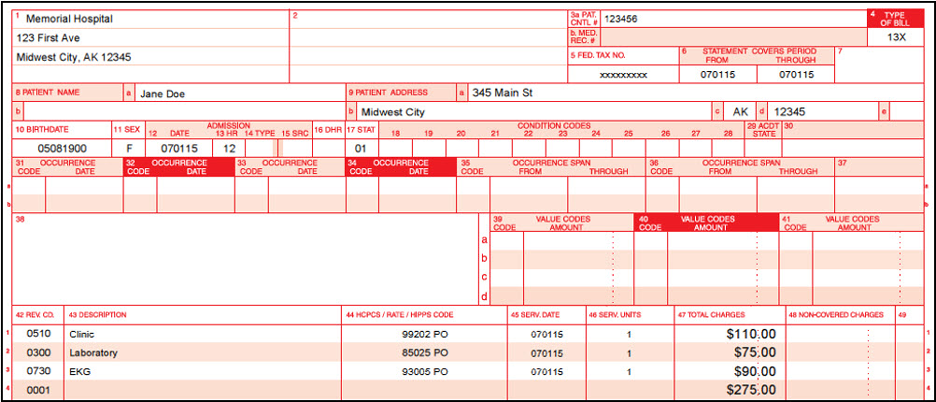
4 Type of Bill M The UB-04 claim form may be used to bill for inpatient hospital care or to replace a claim for inpatient hospital care that was paid by MA. Enter the appropriate three-digit code to identify the type of bill being submitted. The format of the three-digit code is indicated below: 1. First digit: Type of facility – always enter
What is a facility billing form?
Section 3004 of the Affordable Care Act CMS has created a website to support Section 3004 of the Affordable Care Act, Quality Reporting for Long Term Care Hospitals, Inpatient Rehabilitation Hospitals and Hospice Programs. This site has been created so that the public can view information, and communications, related to Section 3004.
What does Medicare Part a cover for rehab?
We bill for an outpatient drug and alcohol rehab facility that is owned by an LCSW. Some insurance carriers have it credentialed as a facility and require the billing to be done on UB04 forms. This is beneficial to our client because the facility reimbursement rate is higher than the professional reimbursement rate.
When will I be admitted to an inpatient rehabilitation facility?
Mar 01, 2020 · The IRF-PAI form helps compensate for inpatient care with a predetermined revenue amount from the RA-scored diagnosis related to the rehab patient’s documented treatment. The IRF-PAI form completion and staff documentation supports the case mix, POA diagnosis, HCC-RA ratings for each disease, and associated comorbidities.
What is Bill Type 22x?
Bill type 22x is used for those SNF residents who are in non-covered stays but are placed in the Medicare-certified distinct part of the institution.May 9, 2003
Which payment system is used for inpatient rehabilitation facilities?
The Medicare program in 2002 instituted an inpatient rehabilitation facility (IRF) prospective payment system (PPS). IRFs are specialized hospitals or hospital units that provide intensive rehabilitation in an inpatient setting.
How do I bill Medicare for physical therapy?
You must complete at least eight minutes of treatment be paid for one 15-minutes increment. So, for example, if you completed 17 minutes of treatment, Medicare would be billed for 15 minutes, or one unit. However, if you completed 23 minutes of treatment, Medicare would be billed for two units of treatment.Nov 1, 2019
How are IRF reimbursed?
Payment for IRFs is on a per discharge basis, with rates based on such factors as patient-case mix, rehabilitation impairment categories and tiered case-mix groups. Rates may be adjusted based on the length of stay, geographic area and demographic group.
What is prospective payment system in healthcare?
A Prospective Payment System (PPS) is a method of reimbursement in which Medicare payment is made based on a predetermined, fixed amount. The payment amount for a particular service is derived based on the classification system of that service (for example, diagnosis-related groups for inpatient hospital services).Dec 1, 2021
What are the CMS 13 diagnosis?
Understanding qualifying conditions for admissionStroke.Spinal cord injury.Congenital deformity.Amputation.Major multiple trauma.Fracture of femur.Brain injury.Neurological disorders.More items...
What is the Revenue Code for physical therapy?
420Occupational,Physical and Speech TherapyRevenue CodeDescription420Physical therapy421Visit charge422Hourly charge423Group rate14 more rows•Mar 18, 2021
What is the CPT code for physical therapy?
CPT codes are used to classify medical, surgical and diagnostic services and procedures, and range from 00100 to 99499....The Most Common Physical Therapy CPT codes:97110Therapeutic Exercise97140Manual Therapy97112Neuromuscular Re-Education97530Therapeutic Activities26 more rows•Aug 2, 2019
What is KY modifier used for?
The KY Modifier is used to identify a wheelchair accessory that is for use with a base that was not part of the competitive bid program. This modifier is only for use in former competitive bid areas and is important to ensure appropriate pricing on the wheelchair accessories.
How are LTACHs reimbursed?
Once so designated, LTACHs are reimbursed through specific long-term care DRGs (LTC-DRGs). These LTC-DRGs have the same definitions as the short-term acute DRGs but, to compensate for longer staying patients, these facilities have much higher relative weights applied to a higher base rate payment.Mar 22, 2021
What are some CMS criteria for inpatient rehabilitation facilities?
Recently, the Centers for Medicare & Medicaid Services (CMS) advised its medical review contractors that when the current industry standard of providing in general at least 3 hours of therapy (physical therapy, occupational therapy, speech-language pathology, or prosthetics/orthotics) per day at least 5 days per week ...Dec 20, 2018
What format do you use for a patient who is unable to work?
If the patient is currently employed but is unable to work due to this condition, record the dates that the patient wasn’t able to work in the MM DD YYYY format. If this condition doesn’t affect the patient’s ability to work, leave this field blank.
What does item 12 mean in a medical claim?
In item 12, include the patient’s (or authorized person’s) legal signature—or input “Signature on File” or “SOF”—and the sign date (MM/DD/YYYY) to indicate that the patient (or an authorized person) has authorized the release of his or her medical information to process the claim.
What is the modifier for MMDDYYYYY?
Input the first onset date (MM DD YYYY) of the current illness or injury. Then, after the date, include modifier 431 to indicate that date represents the onset of the patient’s current illness or injury.
Where is the modifier Y4 on a workers comp claim?
If submitting a claim to a property or casualty payer (e.g., homeowners or workers’ comp), input the correct modifier (Y4) to the left of the vertical dotted line and the relevant claim casualty number to the right. If this is not applicable, leave this section blank.
How to indicate whether or not lab services were rendered by an independent provider?
Use this field to indicate whether or not lab services were rendered by an independent provider. If you mark “YES,” then include the dollar amount for the charges. Do not use commas, a decimal point, or a dollar sign. If the amount charged is a whole number, add “00” to the end of the number to represent cents.
When was the 1500 form introduced?
CMS-1500 forms were introduced in the 1980s to help standardize healthcare claims on a national level—and now, according to the National Uniform Claim Committee (NUCC), “the 1500 Claim Form is accepted nationwide by most insurance entities as the standard claim form/attending physician statement for submission of medical claims.” But as helpful as the CMS-1500 form was for aiding standardization, the paper version is starting to become a claim form of the past. Many modern electronic billing software and solutions eschew paper claims altogether, and help providers send the same claims without the hassle of filling out complicated, long-form paperwork.
Can you fill out a CMS-1500 by hand?
Ensure that the printer cartridge does not leak, smudge, smear, or create any excess lines on the claim. Ensure that none of the printed characters touch. You can, of course, complete your CMS-1500 forms by hand, but they will typically take longer to process than those that are typed.
What is section 3004?
Section 3004 of the Affordable Care Act. CMS has created a website to support Section 3004 of the Affordable Care Act, Quality Reporting for Long Term Care Hospitals, Inpatient Rehabilitation Hospitals and Hospice Programs.
When will CMS 1748-P be released?
CMS-1748-P: Medicare Program; Inpatient Rehabilitation Facility Prospective Payment System for Federal Fiscal Year 2022 and Updates to the IRF Quality Reporting Program is on public display at the Office of Federal Register and will publish on April 12, 2021. The rule and associated wage index file is available on the web page
What is facility billing?
Facility billing is insurance billing for hospitals, inpatient or outpatient clinics, and other offices such as ambulatory surgery centers. This insurance billing is not the same as billing for a regular doctor or specialist.
Do insurance carriers require UB04?
Some insurance carriers have it credentialed as a facility and require the billing to be done on UB04 forms. This is beneficial to our client because the facility reimbursement rate is higher than the professional reimbursement rate. But other insurance carriers will not credential him as a facility and he must bill services out to them on CMS 1500 ...
Is the book "The Littler Guy" hard to navigate?
The book is hard to navigate and is actually quite costly. The information in it is required if you are doing in depth inpatient billing, but for the littler guy, such as outpatient clinics, it is too much info and too difficult to decipher.
Do you need a rev code for UB04?
For example, UB04 forms require rev codes and a type of bill code that are not required on the CMS1500 form. There are also a lot of "conditional fields" that for most situations are not required to be completed.
What is inpatient rehab coding?
Inpatient rehab coding involves reading proper, clear documentation, as well as skillful, accurate, and detailed abstraction of the POA diagnosis code, sequela effects, ongoing comorbidities, forever diagnosis codes, chronic conditions, use of assistive devices, and complications.
What is POA in IRF?
The IRF physicians and clinical support staff must document to prove medical necessity for treating the principal diagnosis on admission (POA), as well as the ongoing comorbidities.
What is the coding system used for outpatient rehabilitation?
The HCPCS is the coding system used for the reporting of these services.
What is Medicare Part B therapy?
Under the MPFS (Medicare Part B), Medicare pays for services provided by physicians and practitioners that are specifically authorized by statute. Students do not meet the definition of practitioners under Medicare Part B. Under SNF PPS, payments are based upon the case mix or RUG category that describes the patient. In the rehabilitation groups, the number of therapy minutes delivered to the patient determines the RUG category. Payment levels for each category are based upon the costs of caring for patients in each group rather than providing specific payment for each therapy service as is done in Medicare Part B
What is the HCPCS code for occupational therapy?
beneficiary received occupational therapy (HCPCS code 97530 which is defined in 15 minute intervals) for a total of 60 minutes. The provider would then report revenue code 043X in FL 42, HCPCS code 97530 in FL 44, and 4 units in FL 46.
What is the CMS 1450?
Effective with claims submitted on or after April 1, 1998, providers billing on Form CMS-1450 are required to report the number of units for outpatient rehabilitation and certain audiology services based on the procedure or service , e.g., based on the HCPCS code reported instead of the revenue code. This was already in effect for billing on the Form CMS-1500. CORFs report their full range of CORF services on the Form CMS-1500. Units are reported based on the number of times the procedure, as described in the HCPCS code definition, is performed. When reporting service units for HCPCS codes where the procedure is not defined by a specific timeframe, the provider enters “1” in units. Since providers may perform a number of procedures or services during a single visit, the number of units may exceed the number of visits. Visits should not be reported as units for these services.
Do OPTs bill for supplies?
OPTs should not bill for the supplies they furnish. Since supplies are part of the practice expense, under the MPFS these expenses are already taken into account in the practice expense relative values.
Can a therapist be billed under Medicare?
Only the services of the therapist can be billed and paid under Medicare Part B. The services performed by a student are not reimbursed even if provided under “line of sight” supervision of the therapist; however, the presence of the student “in the room” does not make the service unbillable. Pay for the direct (one-to-one) patient contact services of the physician or therapist provided to Medicare Part B patients. Group therapy services performed by a therapist or physician may be billed when a student is also present “in the room”.
Do carriers pay for outpatient therapy?
Carriers pay for outpatient physical therapy services (which includes outpatient speech-language pathology services) and outpatient occupational therapy services provided simultaneously to two or more individuals by a practitioner as group therapy services. The individuals can be, but need not be performing the same activity. The physician or therapist involved in group therapy services must be in constant attendance, but one-on-one patient contact is not required.
What is part A in rehabilitation?
Inpatient rehabilitation care. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
How long does it take to get into an inpatient rehab facility?
You’re admitted to an inpatient rehabilitation facility within 60 days of being discharged from a hospital.
Does Medicare cover private duty nursing?
Medicare doesn’t cover: Private duty nursing. A phone or television in your room. Personal items, like toothpaste, socks, or razors (except when a hospital provides them as part of your hospital admission pack). A private room, unless medically necessary.
Does Medicare cover outpatient care?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
What are the exclusions for Medicare?
The following are excluded from this change: 1 Hospitals with a waiver exempting them from Medicare’s Inpatient Prospective Payment System (IPPS) or the TRICARE DRG-based payment system 2 Children’s and VA hospitals 3 Costs of physician services or other professional services 4 Custodial or domiciliary care, even if rendered in an otherwise authorized LTCH
What is the Medicare PPS for the second 12 months?
For the second 12 months, the TRICARE PPS allowable cost will be 115 percent of the Medicare PPS amounts . For the third 12 months, and subsequent years, the TRICARE PPS allowable cost will be 100 percent of the Medicare PPS amounts.
What is the transition period for TRICARE?
The Defense Health Agency implemented a transition period beginning Oct, 1, 2018 , to buffer the financial impact for LTCHs and IRFs: For the first 12 months, the TRICARE PPS allowable cost will be 135 percent of Medicare PPS amounts. For the second 12 months, the TRICARE PPS allowable cost will be 115 percent of the Medicare PPS amounts.
How long does it take to receive LTCH PPS?
Standard LTCH PPS payment rate: In order to receive the standard LTCH PPS rate, the LTCH admission must occur within one day of a hospital discharge, which includes discharges from military or U.S. Department of Veterans Affairs hospitals.
Learning About The CMS-1500 Form
Following The Formatting Rules
- Just because you’re submitting the CMS-1500 claim form on paper, that doesn’t mean you have to complete the entire form by hand. Some organizations (like the Washington State Department of Labor & Industries) have created digital PDF copies of the CMS-1500 form. However, while typing the claim information will be lightyears faster than writing it a...
Filling Out The Form—Field by Field
- Now that you’ve finished prepping, it’s time to dig into the meat and potatoes of the form-filling experience: inputting claim info. I’m going to go field by field and explain exactly what needs to go where—and how it needs to look, based on the instructions published by the NUCC.