What is the meaning of re rehabilitation?
Nov 10, 2021 · The benefits of rehabilitation. Rehabilitation can reduce the impact of a broad range of health conditions, including diseases (acute or chronic), illnesses or injuries. It can also complement other health interventions, such as medical and surgical interventions, helping to achieve the best outcome possible.
When do I have to pay a deductible for rehabilitation?
Aug 19, 2014 · Severe aortic or mitral stenosis (aortic or mitral valve area <1.0cm2 or mean gradient > 40 mmHg or > 10 mmHg respectively) Dynamic left ventricular (LV) outflow obstruction. Patients who have demonstrated exercise induced ventricular arrhythmias or have experienced a recent hospitalization for arrhythmias.
What is the CPT code for psychiatric reduction?
Days 1-60: $1,556 deductible.*. Days 61-90: $389 coinsurance each day. Days 91 and beyond: $778 coinsurance per each “lifetime reserve day” after day 90 for each benefit period (up to a maximum of 60 reserve days over your lifetime). Each day after the lifetime reserve days: All costs. *You don’t have to pay a deductible for inpatient ...
What happens in drug rehab?
Oct 12, 2017 · Per IOM 100-02, Chapter 15, Section 232, “Cardiac rehabilitation (CR) services mean a physician-supervised program that furnishes physician prescribed exercise, cardiac risk factor modification, including education, counseling, and behavioral intervention; psychosocial assessment, outcomes assessment, and other items/services as determined by the Secretary …
What are the 4 pillars of harm reduction?
The Four Pillars approach is recognized internationally as an effective way to address the harms associated with substance use. It uses the four pillars of Prevention, Harm Reduction, Enforcement, and Treatment to form a balanced, solid foundation on which to build a comprehensive community drug strategy.
What is harm reduction in behavioral health?
policies, programmes and practices that aim primarily to reduce the adverse health, social and economic consequences of the use of legal and illegal psychoactive drugs without necessarily reducing drug consumption. Harm reduction benefits people who use drugs, their families and the community.” [27].Oct 24, 2017
What are the 5 stages of rehab?
Don't Forget the RehabPhase 1 - Control Pain and Swelling.Phase 2 - Improve Range of Motion and/or Flexibility.Phase 3 - Improve Strength & Begin Proprioception/Balance Training.Phase 4 - Proprioception/Balance Training & Sport-Specific Training.Phase 5 - Gradual Return to Full Activity.
What is harm reduction CDC?
Harm reduction is any behavior or strategy that helps reduce risk or harm to yourself or others. For example, to reduce the risk of contracting or transmitting HIV, you can practice safer sex or safer drug use.
What is a harm reduction specialist?
The Harm Reduction Specialist provides engagement and support services, particularly to program participants engaging in behaviors that may pose risks such as drug and alcohol use, sexual practices, and self-injury, using a harm reduction approach.
Whats a harm reduction kit?
The harm reduction program provides sterile, single-use injection and inhalation supplies and safe disposal of used drug equipment: Clean syringes. Alcohol swabs. Sterile water. Tourniquets.
What are the 3 P's of recovery?
3 “P's” for Recovery: Passion, Power and Purpose.Aug 18, 2016
What are the 3 phases of rehabilitation?
Athletic trainers (ATs) have traditionally conceptualized rehabilitation programs in terms of 3 distinct physiologic phases: acute injury phase, repair phase, and remodeling phase.
How long is physical reconditioning?
A licensed physical therapist and strength coach will supervise the program. An average program can last anywhere from a couple of weeks to a few months, depending on the needs of the individuals in the group.
What is total abstinence?
While stimulant addicts are of course at the highest risk when using stimulants, “total abstinence” means avoiding other psychoactive substances as well.
What is part A in rehabilitation?
Inpatient rehabilitation care. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
How long does it take to get into an inpatient rehab facility?
You’re admitted to an inpatient rehabilitation facility within 60 days of being discharged from a hospital.
What is the benefit period for Medicare?
benefit period. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services. A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row.
Does Medicare cover private duty nursing?
Medicare doesn’t cover: Private duty nursing. A phone or television in your room. Personal items, like toothpaste, socks, or razors (except when a hospital provides them as part of your hospital admission pack). A private room, unless medically necessary.
Does Medicare cover outpatient care?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, Section 1833 (e) states that no payment shall be made to any provider of services or other person under this part unless there has been furnished such information as may be necessary in order to determine the amounts due such provider or other person under this part for the period with respect to which the amounts are being paid or for any prior period..
Article Guidance
History/Background and/or General Information:#N#It has come to Novitas’ attention that providers who are not physicians (MD or DO) are prescribing (i.e.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is Medicare IRF?
All hospitals or units of a hospital that are classified under subpart B of part 412 of the Medicare regulations as inpatient rehabilitation facilities (IRFs). Medicare payments to IRFs are based on the IRF prospective payment system (PPS) under subpart P of part 412.
When was the 412.23(b)(2) review suspended?
On June 7 , 2002, CMS notified all ROs and FIs of its concerns regarding the effectiveness and consistency of the review to determine compliance with §412.23(b)(2). As a result of these concerns, CMS initiated a comprehensive assessment of the procedures used by the FIs to verify compliance with the compliance percentage threshold requirement and suspended enforcement of the compliance percentage threshold requirement for existing IRFs. The suspension of enforcement did not apply to a facility that was first seeking classification as an IRF in accordance with §412.23(b)(8) or §412.30(b)(2). In such cases, all current regulations and procedures, including §412.23(b)(2), continued to be required.
What is Medicare certified hospital?
Section 1886(d)(1)(B) of the Social Security Act (the Act) and Part 412 of the Medicare regulations define a Medicare certified hospital that is paid under the inpatient (acute care hospital) prospective payment system (IPPS). However, the statute and regulations also provide for the classification of special types of Medicare certified hospitals that are excluded from payment under the IPPS. These special types of hospitals must meet the criteria specified at subpart B of Part 412 of the Medicare regulations. Failure to meet any of these criteria results in the termination of the special classification, and the facility reverts to an acute care inpatient hospital or unit that is paid under the IPPS in accordance with all applicable Medicare certification and State licensing requirements. In general, however, under §§ 412.23(i) and 412.25(c), changes to the classification status of an excluded hospital or unit of a hospital are made only at the beginning of a cost reporting period.
What is 412.23(b)(2)?
Under revised §412.23(b)(2), a specific compliance percentage threshold of an IRF’s total patient population must require intensive rehabilitation services for the treatment of one or more of the specified conditions. Based on the final rule, CMS issued a Joint Signature Memorandum including instructions related to Regional Office (RO) and Medicare fiscal intermediary (FI) responsibilities regarding the performance of reviews to verify compliance with §412.23(b)(2) as detailed in CRs 3334 and 3503, which revised Medicare Claims Processing Manual Chapter 3, sections 140.1 to 140.1.8. (CR 3503 corrected some errors or clarified the instructions in CR 3334 and presented additional instructions to implement revised §412.23(b)(2).
When was the CMS rule for major multiple traumas?
In the proposed rule dated September 9, 2003 (FR 68, 53272) CMS clarified which patients should be counted in the category of major multiple traumas to include patients in diagnosis-related groups 484, 485, 486 or 487 used under the IPPS.
What is the intake process for drug rehab?
The intake process for drug rehab usually involves a medical assessment and an orientation to the facility. The process can be lengthy and involved, but the information the treatment team collects during intake will set you up for success.
What is Amy's role in addiction?
Amy is an advocate for patient- and family-centered care. She previously participated in Moffitt Cancer Center’s patient and family advisory program and was a speaker at the Institute of Patient-and Family-Centered Care’s 2015 national conference.
What happens after a drug intake interview?
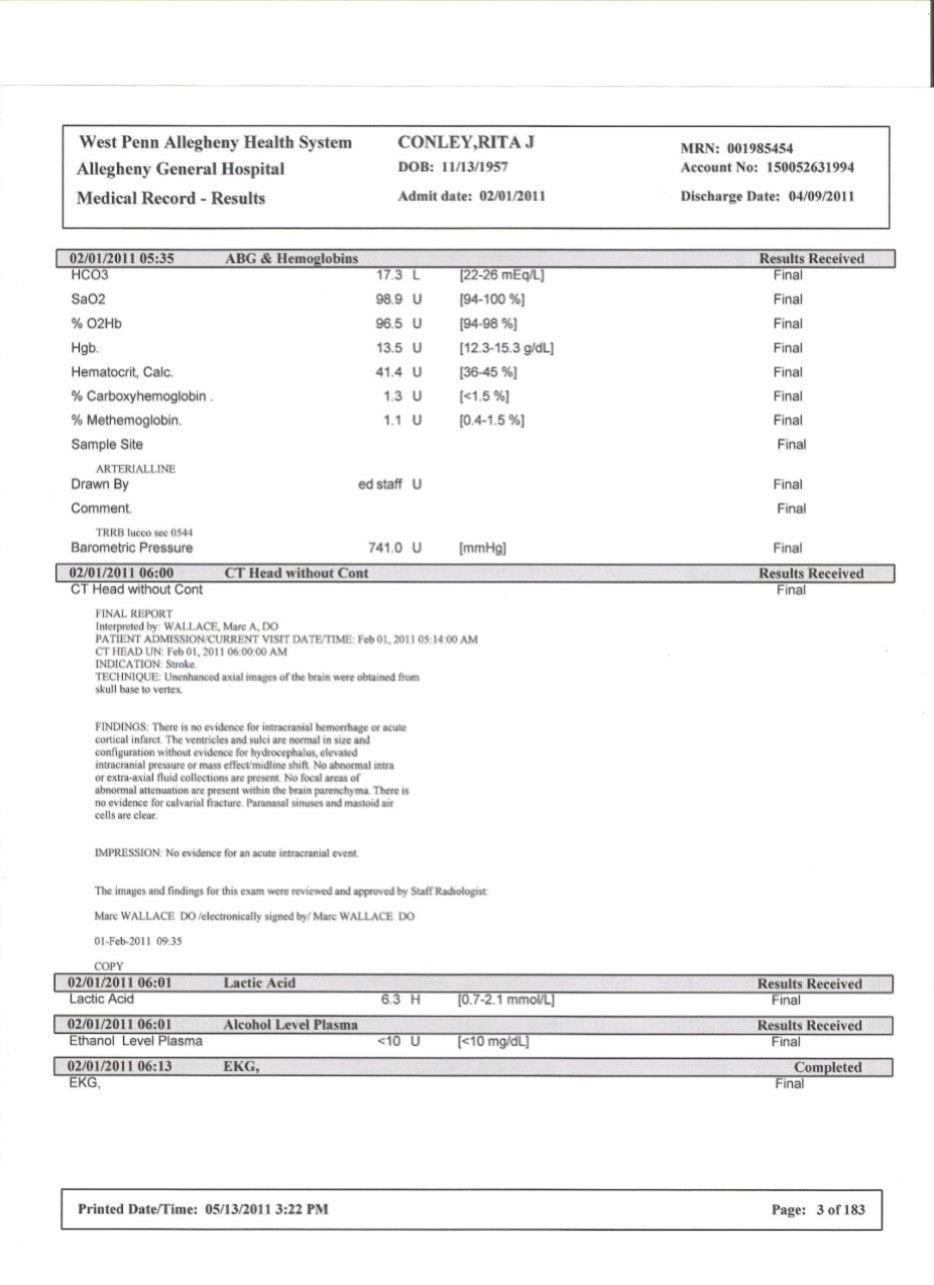
After intake interviews are complete, you’ll likely undergo an in-depth medical evaluation, including blood, urine and other lab tests to assess your health and the severity of your drug use. If no drugs or alcohol are present in your system, you may be transferred directly into a behavioral therapy program.
What is a reason code used on an EOB?
Reason codes appear on an explanation of benefits (EOB) to communicate why a claim has been adjusted. If there is no adjustment to a claim/line, then there is no adjustment reason code.
Here is a comprehensive reason codes list
Do you have reason code with you? Want to know what is the exact reason?
Medical Billers And Coders - Credentialing Services
Simplifying Every Step of Credentialing Process, Most trusted and assured Credentialing services for all you need, like Physician Credentialing Services, Group Credentialing Services, Re-Credentialing Services, Additionally We do provide:
What is rehabbing a house?
One of the more costly projects a real estate investor can undertake is rehabbing houses. This endeavor can be both daunting and challenging, especially for beginner investors, as it consists of purchasing a property, renovating it, and selling it for full market value. Rehabbing requires attention to detail and a lot of time to master, ...
What is the difference between a fixer upper and a rehab?
The best way to think about a house rehab vs. fixer-upper is overall workload and cost: a house rehab is typically a more comprehensive project than a fixer-upper. House rehabs will involve renovating the property and making bigger changes, like fixing electrical, plumbing, or roofing issues. On the other hand, a fixer-upper typically focuses on cosmetic changes that can be made quickly or at a lower cost than a full rehab. A good rule of thumb is that if someone can live in the property during renovations, it will most likely be a fixer-upper and not a full house rehab.
What are lender fees?
Lender Fees: Depending on how the property is financed, different lender fees could be required. More often than not, these will cover paperwork, title searches, and other costs associated with property purchase. Ownership Costs: Do not forget to account for holding costs when estimating the overall budget.
What is the last piece of work to do when rehabbing a house?
The last piece to rehabbing a house on a budget is finalizing the improvements. With the contractor by your side, you must examine all of the work done, including double-checking any adjustments made during the renovation. A final inspection by a professional service is also recommended, as they can essentially confirm the work completed by the contractor is up to par with standards.
Why is it important to find a good contractor for rehab?
These individuals will play a crucial role in transforming your property into a winning investment. However, not all contractors are created equal. Investors will need to spend a responsible amount of time researching general contractors. This meticulous process will help investors steer clear of bad contractors, ultimately costing time, patience, and money.
Is it okay to walk away from a deal?
Not knowing when to walk away: It is okay to walk away from a potential deal if something is not right. For example, don’t be afraid to pass up on a property if you cannot find the right financing or team. These details can greatly impact the success of the project, even if the other details seem perfect.
What is included in a home inspection?
In most cases, a home inspection will include examining the home’s heating and air-conditioning system, electrical system, plumbing, foundation, roof, flooring, walls, ceilings, windows, doors, and insulation. As an investor, it’s important to take a combination of notes and pictures during the initial inspection.
Brain Injury
Brain injury: (Liu, 2004; n=175 with n=101 with vascular brain injury, n=49 with traumatic brain injury, n=27 with other brain injuries; median age=45, inpatient rehabilitation; length of stay=95 days).
Non-Specific Patient Population
Inpatient rehab: (Castiglia et al., 2017; n=53; mean age 72.71 (12.79); orthopedic diseases n=21; PD or stroke n=32; mean hospital duration: 45.11 (16.53) days, Italian version)
Older Adults and Geriatric Care
Older Adults in Nursing Homes: (Bouwstra et al., 2018; n=244; mean age: 77 (9.7) Years, Collin and Wade’s BI)
Stroke
Chronic Stroke: (Hsieh et al, 2007; n = 56; mean time post-stroke = 1197.1 (1281.8) days; mean age = 59.4 (14.6) years; Taiwanese sample)
Parkinson's Disease
Parkinson’s Disease: (Taghizadeh, et al., 2019; n = 260, mean age = 60.3 (12.3) years; female=28.1%; Mean time since diagnosis (SD): 6.6 (5.5); Stage 1: 33.9%; Stage 2: 36.5%; Stage 3: 20%; Stage 4: 9.6%, Iranian version)
More Instruments Like This
We have reviewed nearly 300 instruments for use with a number of diagnoses including stroke, spinal cord injury and traumatic brain injury among several others.