The shift note summarizes patient education, safety, therapy carry over, medical concerns, etc. Things that justify the need for 24-hour rehab nursing. So... think of an auditor reviewing the note for appropriateness and if your note says - call light within reach, no problems, etc... they'll say - why did this patient need acute rehab?
Full Answer
How do you code inpatient rehab?
Mar 03, 2013 · The shift note summarizes patient education, safety, therapy carry over, medical concerns, etc. Things that justify the need for 24-hour rehab nursing. So... think of an auditor reviewing the note for appropriateness and if your note says - call light within reach, no problems, etc... they'll say - why did this patient need acute rehab?
What is the format of a patient note for Medicare?
This item: Rehab Notes: A Clinical Examination Pocket Guide. by Ellen Z. Hillegass PT PhD Spiral-bound . $29.99. Only 1 left in stock - order soon. Ships from and sold by nagpurkar. $4.98 shipping. Ortho Notes: Clinical Examination Pocket Guide. by …
What is inpatient rehabilitation and how does it work?
HOSPITAL DISCHARGE PREPARATION CHECKLIST BEFORE DAY OF DISCHARGE, UNDERSTAND: What equipment is to be ordered? Equipment preparation req'd? Who is placing the order?
What does Medicare say about rehabilitation therapy?
1. Rehabilitation: The patient continues to participate fully in all therapy sessions. She requires cues for attending to the left side at times. Continue comprehensive inpatient rehabilitation and discharge planning. 2. Stroke prevention: No new stroke findings. Continue Aggrenox as written. 3. Deep venous thrombosis prevention.

What is the main focus of a rehabilitation hospital?
“The ultimate goal of a rehabilitation hospital is to help patients recover and be able to return to functioning as independently as possible in their homes.” The ultimate goal of a rehabilitation hospital is to help patients recover and be able to return to functioning as independently as possible in their homes.Oct 21, 2020
What are the 3 types of rehab?
The three main types of rehabilitation therapy are occupational, physical and speech. Each form of rehabilitation serves a unique purpose in helping a person reach full recovery, but all share the ultimate goal of helping the patient return to a healthy and active lifestyle.May 23, 2018
What is the purpose of inpatient rehabilitation?
From your first therapy session to your last check-in, the goal of inpatient rehab is to help people with serious medical conditions like stroke, heart failure, joint replacement or serious injury recover faster, as fully as possible.Aug 16, 2018
What are the levels of rehab?
Read on for our rundown of the eight most common rehab settings.Acute Care Rehab Setting. ... Subacute Care Rehab Setting. ... Long-term Acute Care Rehab Setting. ... Home Health Care Rehab Setting. ... Inpatient Care Rehab Setting. ... Outpatient Care Rehab Setting. ... School-Based Rehab Setting. ... Skilled Nursing Facility Rehab Setting.
What are rehab activities?
Activities To Do At Rehab In CaliforniaListening To Music Together. Music is proven to get a shift of the atmosphere, be it joy, tranquility and other emotions to heighten. ... Get A Book To Read. ... Take A Stroll. ... Write A Letter For A Loved One. ... Play A Puzzle Game. ... Use A Coloring Book.Aug 9, 2021
What's another word for rehab?
What is another word for rehab?recoveryrecuperationrehabilitationconvalescencehealingmendingrallycomebacksnapbackrestoration34 more rows
What is the difference between rehab and PT?
Rehabilitation is the process that assists a person in recovering from a serious injury, while physical therapy will help with strength, mobility and fitness.Nov 25, 2016
Is AA and rehab the same thing?
While many rehab facilities do use the tenets of AA in their treatment activities, AA itself does not comprise the full treatment regimen needed for effective rehab. The great thing about AA is that it helps you turn yourself over to a higher power, learn to admit your mistakes, and work on changing your life.Oct 12, 2021
What are the CMS 13 diagnosis?
Understanding qualifying conditions for admissionStroke.Spinal cord injury.Congenital deformity.Amputation.Major multiple trauma.Fracture of femur.Brain injury.Neurological disorders.More items...
What are the 4 types of rehabilitation?
Rehabilitation ElementsPreventative Rehabilitation.Restorative Rehabilitation.Supportive Rehabilitation.Palliative Rehabilitation.
What is level1 rehabilitation?
'Tertiary specialised' rehabilitation services (Level 1) are high cost / low volume services, which provide for patients with highly complex rehabilitation needs following illness or. injury, that are beyond the scope of their local general and specialist services.
What is a rehabilitation setting?
Rehabilitation is defined as “a set of interventions designed to optimize functioning and reduce disability in individuals with health conditions in interaction with their environment”.Nov 10, 2021
What is part A in rehabilitation?
Inpatient rehabilitation care. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
How long does it take to get into an inpatient rehab facility?
You’re admitted to an inpatient rehabilitation facility within 60 days of being discharged from a hospital.
Does Medicare cover outpatient care?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
What is the benefit period for Medicare?
benefit period. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services. A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row.
Does Medicare cover private duty nursing?
Medicare doesn’t cover: Private duty nursing. A phone or television in your room. Personal items, like toothpaste, socks, or razors (except when a hospital provides them as part of your hospital admission pack). A private room, unless medically necessary.
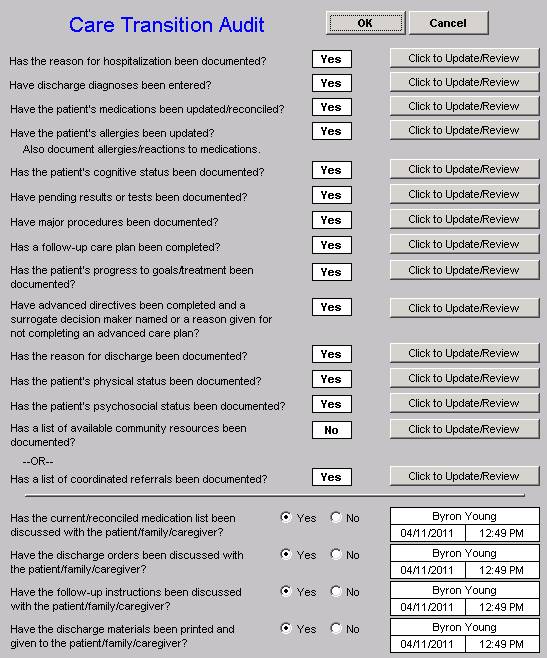
What is an attached document?
The attached document combines all of the clarifications for the IRF coverage requirements into one cohesive document . We believe that this format will make it much easier for IRF providers to find the information they are seeking. Simply clicking on the links at the top of the page will populate the section containing the information on that topic.
What is rehabilitation physician?
The rehabilitation physician is a licensed physician (not necessarily a salaried employee of the IRF) who has specialized training and experience in rehabilitation. It is the responsibility of each IRF to ensure that the rehabilitation physicians that are making the admission decisions and caring for patients are appropriately trained and qualified. While the IRF must continue to meet the hospital conditions of participation specified in 42 Code of Federal Regulations §482.22 regarding documentation of staff qualifications, we do not require specific documentation in the patient’s medical record to demonstrate the rehabilitation physician’s qualifications.
Is IRF coverage necessary?
Instead of using the term “medical necessity,” CMS now refers to appropriate IRF admissions as being “reasonable and necessary.” Thus, the new IRF coverage requirements in the regulations and in section 110 of the Medicare Benefit Policy Manual (Pub. 100-02) define the criteria for an IRF admission to be considered reasonable and necessary.
What is an IRF in nursing?
An IRF must comply with the requirements for nursing set forth in the Hospital Conditions of Participation at 42 CFR §482.23 of the regulations. In addition, the interdisciplinary team must include a registered nurse with specialized training or experience in rehabilitation.
Can IRF patients receive therapy on discharge day?
Generally, we do not expect patients to receive intensive therapies on the day of discharge from the IRF. However, the IRF may provide therapy on the day of discharge if the IRF believes that this is appropriate for the patient.
What is therapy time?
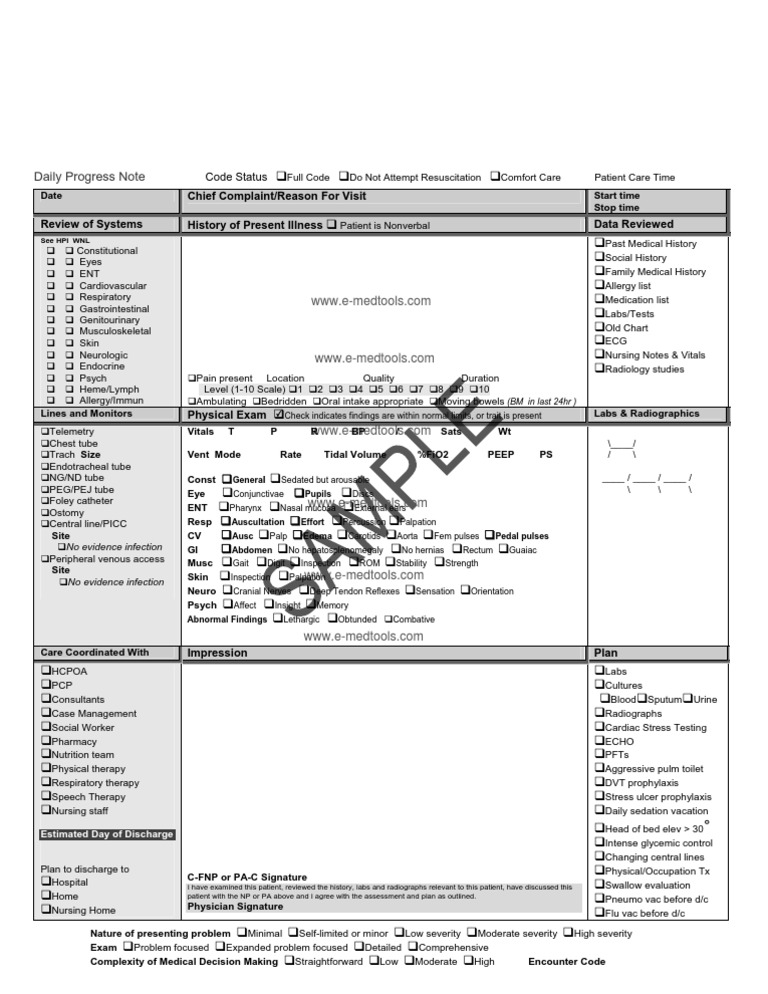
For purposes of demonstrating the intensity of therapy requirement, “therapy time” is time spent in direct contact with the patient. Time spent documenting in the patient’s medical record, unsupervised modalities, and significant periods of rest are examples of time not spent in direct contact with the patient and, therefore, may not be used to demonstrate the intensity of therapy requirement.
What are the IRF coverage requirements for Medicare?
The new IRF coverage requirements permit Medicare’s contractors to grant brief exceptions (not to exceed 3 consecutive calendar days) to the intensity of therapy requirements for unexpected clinical events that limit a patient’s ability to participate in therapy for a limited number of days. For example, if a patient’s plan of care for a particular week calls for the patient to receive a specified number of hours of therapy on Monday, Tuesday, Wednesday, Thursday, and Friday of that week, but the patient experiences an unexpected clinical event on Sunday night that limits the patient’s ability to participate in therapy on Monday and Tuesday, Medicare’s contractors are authorized to allow a brief break in the provision of therapy services on Monday and Tuesday of that week, as long as the reasons for the break in therapy are well-documented in the patient’s medical record at the IRF. Since the provision of therapies on Saturday and Sunday were not part of this particular patient’s plan of care for that week, this example would illustrate a 2 day break in the provision of the patient’s intensive rehabilitation therapy program.
What is ADL in healthcare?
While providing quality care, skilled clinicians must assess the patient’s activities of daily living (ADL) functions in the presence of illness. They must also justify the patient’s etiology for complications and comorbidities in the medical record.
Who is Tamara Thivierge?
Tamara Thivierge, MHA, CPC, is a certified medical coder with over 25 years of broad professional history in diverse settings, including inpatient rehab, behavioral health center, family physicians, and auditing with an insurance payer. She has also led workshops on billing in the Hampton Roads, Va., area.
What is inpatient rehab coding?
Inpatient rehab coding involves reading proper, clear documentation, as well as skillful, accurate, and detailed abstraction of the POA diagnosis code, sequela effects, ongoing comorbidities, forever diagnosis codes, chronic conditions, use of assistive devices, and complications.