This means that a Medicare beneficiary can receive Medicare Part A SNF coverage without a qualifying 3-day hospital inpatient stay if they develop a need for a SNF level of care and could be admitted directly from the community, a doctor’s office, an emergency room, from a hospital observation stay, or from a hospital inpatient stay that is less than 3-days. It also means that a SNF long-term resident could qualify for SNF benefits, or “skill-in-place” without leaving the SNF. Additionally, under the benefit period waiver, this means that a beneficiary could qualify for an additional 100-day benefit period without starting or completing a 60-day break in spell-of-illness, but only if all other Medicare SNF coverage requirements are met.
Full Answer
What is the 3-day rule for Medicare rehab?
Mar 07, 2022 · The 3-day rule for Medicare requires that you are admitted to the hospital as an inpatient for at least 3 days for rehab in a skilled nursing facility to be covered. You must be officially admitted to the hospital by a doctor’s order to even be considered an inpatient, so watch out for this rule. In cases where the 3-day rule is not met, Medicare may cover outpatient rehab. …
How long does Medicare pay for inpatient rehab?
You must pay the inpatient hospital deductible for each benefit period. There's no limit to the number of benefit periods. : Days 1-60: $1,556 deductible.*. Days 61-90: $389 coinsurance each day. Days 91 and beyond: $778 coinsurance per each “lifetime reserve day” after day 90 for each benefit period (up to a maximum of 60 reserve days over ...
Does Medicare pay for rehab in a skilled nursing facility?
Dec 01, 2021 · under the 3-day (or 1-day) payment window policy, all outpatient diagnostic services furnished to a medicare beneficiary by a hospital (or an entity wholly owned or operated by the hospital), on the date of a beneficiary's admission or during the 3 days (1 day for a non-subsection (d) hospital) immediately preceding the date of a beneficiary's …
How long can you stay out of the hospital on Medicare?
Aug 06, 2020 · Medicare covers inpatient rehabilitation care in a skilled nursing facility only after a 3-day inpatient stay at a Medicare-approved hospital. …

How long does it take to get into an inpatient rehab facility?
You’re admitted to an inpatient rehabilitation facility within 60 days of being discharged from a hospital.
What is the benefit period for Medicare?
benefit period. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services. A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row.
What is part A in rehabilitation?
Inpatient rehabilitation care. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
Does Medicare cover private duty nursing?
Medicare doesn’t cover: Private duty nursing. A phone or television in your room. Personal items, like toothpaste, socks, or razors (except when a hospital provides them as part of your hospital admission pack). A private room, unless medically necessary.
Does Medicare cover outpatient care?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
Implementation of New Statutory Provision Pertaining to Medicare 3-Day (1-Day) Payment Window Policy - Outpatient Services Treated As Inpatient
On June 25, 2010, President Obama signed into law the “Preservation of Access to Care for Medicare Beneficiaries and Pension Relief Act of 2010,” Pub. L. 111-192.
Background
Section 1886 (a) (4) of the Act, as amended by the Omnibus Budget Reconciliation Act of 1990 (OBRA 1990, Pub. L. 101-508), defines the operating costs of inpatient hospital services to include certain outpatient services furnished prior to an inpatient admission.
How long does Medicare require for rehabilitation?
In some situations, Medicare requires a 3-day hospital stay before covering rehabilitation. Medicare Advantage plans also cover inpatient rehabilitation, but the coverage guidelines and costs vary by plan. Recovery from some injuries, illnesses, and surgeries can require a period of closely supervised rehabilitation.
How many hours of therapy per day for rehabilitation?
access to a registered nurse with a specialty in rehabilitation services. therapy for at least 3 hours per day, 5 days per week (although there is some flexibility here) a multidisciplinary team to care for you, including a doctor, rehabilitation nurse, and at least one therapist.
What to do if you have a sudden illness?
Though you don’t always have advance notice with a sudden illness or injury, it’s always a good idea to talk with your healthcare team about Medicare coverage before a procedure or inpatient stay, if you can.
How long does it take for a skilled nursing facility to be approved by Medicare?
Confirm your initial hospital stay meets the 3-day rule. Medicare covers inpatient rehabilitation care in a skilled nursing facility only after a 3-day inpatient stay at a Medicare-approved hospital. It’s important that your doctor write an order admitting you to the hospital.
What are the conditions that require inpatient rehabilitation?
Inpatient rehabilitation is often necessary if you’ve experienced one of these injuries or conditions: brain injury. cancer. heart attack. orthopedic surgery. spinal cord injury. stroke.
How many days do you have to stay in the hospital for observation?
If you’ve spent the night in the hospital for observation or testing, that won’t count toward the 3-day requirement. These 3 days must be consecutive, and any time you spent in the emergency room before your admission isn’t included in the total number of days.
Does Medicare cover knee replacement surgery?
The 3-day rule does not apply for these procedures, and Medicare will cover your inpatient rehabilitation after the surgery. These procedures can be found on Medicare’s inpatient only list. In 2018, Medicare removed total knee replacements from the inpatient only list.
How long is an inpatient in Medicare?
Medicare considers a patient to be in inpatient status if that patient is anticipated to need to be in the hospital for 2 midnights and in observation status if the patient is anticipated to be in the hospital for less than 2 midnights. Observation status was originally intended to be used to observe the patient to determine whether ...
How many days prior to SNF for Medicare?
However, for SNF coverage decisions, Medicare will not count the 3 days prior to the inpatient order toward the 3 inpatient days that Medicare requires in order for Medicare to pay for SNF charges. Medicare’s coverage rules are byzantine and indecipherable for the average patient.
How long does it take for Medicare to pay for SNF?
The 3-day rule is Medicare’s requirement that a patient has to be admitted to the hospital for at least 3 days in order for Medicare to cover the cost of a SNF after the hospitalization. If the patient is admitted for less than 3 days, then the patient pays the cost of the SNF and Medicare pays nothing. So, if this patient was in the hospital ...
How long does it take for a surgeon to change an order to inpatient?
The surgeon writes an order for the patient to be in observation status at the time of the surgery. After 2 days , the surgeon changes the order to inpatient status. The patient spends 4 nights in the hospital but still need more rehabilitation so the patient is discharged to a SNF.
How long do you have to stay in the hospital after a heart surgery?
The patient has difficult-to-control diabetes, heart failure, sleep apnea, and kidney failure so the surgeon anticipates that the patient will need to stay in the hospital for more than 2 midnights after the surgery to care for the medical conditions.
How long does a patient stay in the hospital with pneumonia?
The patient stays in the hospital for 5 days (all 5 in inpatient status) and gets discharged to a SNF.
How long was a woman in the hospital after knee replacement?
She was in the hospital for 4 days after her surgery but was very slow to recover and was determined to be unsafe for discharge home without additional rehabilitation so she was discharged to a SNF (subacute nursing facility). She spent a week getting rehab at the SNF and then returned home only to find that she had a bill for the entire stay the nursing facility; Medicare covered none of it. She paid her bills but in doing so, wiped out most of her savings.
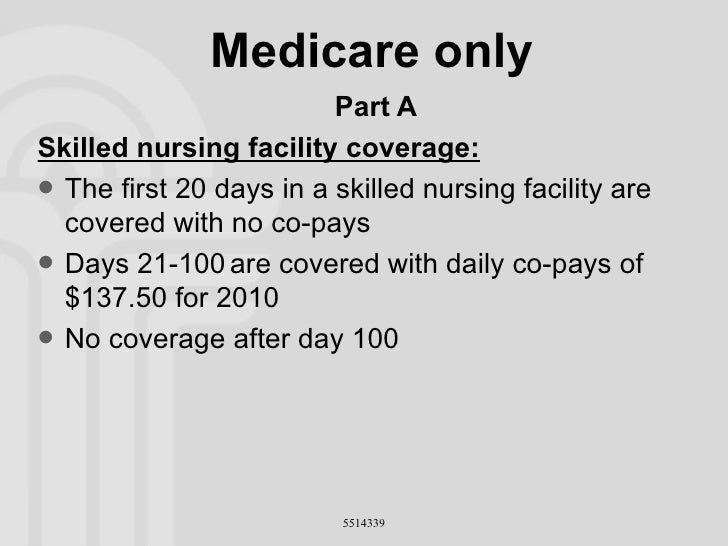
How long does rehab last in a skilled nursing facility?
When you enter a skilled nursing facility, your stay (including any rehab services) will typically be covered in full for the first 20 days of each benefit period (after you meet your Medicare Part A deductible). Days 21 to 100 of your stay will require a coinsurance ...
How long does Medicare cover SNF?
After day 100 of an inpatient SNF stay, you are responsible for all costs. Medicare Part A will also cover 90 days of inpatient hospital rehab with some coinsurance costs after you meet your Part A deductible. Beginning on day 91, you will begin to tap into your “lifetime reserve days.".
How much is Medicare Part A deductible for 2021?
In 2021, the Medicare Part A deductible is $1,484 per benefit period. A benefit period begins the day you are admitted to the hospital. Once you have reached the deductible, Medicare will then cover your stay in full for the first 60 days. You could potentially experience more than one benefit period in a year.
How much is coinsurance for inpatient care in 2021?
If you continue receiving inpatient care after 60 days, you will be responsible for a coinsurance payment of $371 per day (in 2021) until day 90. Beginning on day 91, you will begin to tap into your “lifetime reserve days,” for which a daily coinsurance of $742 is required in 2021. You have a total of 60 lifetime reserve days.
What day do you get your lifetime reserve days?
Beginning on day 91 , you will begin to tap into your “lifetime reserve days.". You may have to undergo some rehab in a hospital after a surgery, injury, stroke or other medical event. The rehab may take place in a designated section of a hospital or in a stand-alone rehabilitation facility. Medicare Part A provides coverage for inpatient care ...
How long do you have to be out of the hospital to get a deductible?
When you have been out of the hospital for 60 days in a row, your benefit period ends and your Part A deductible will reset the next time you are admitted.
Does Medicare cover outpatient treatment?
Medicare Part B may cover outpatient treatment services as part of a partial hospitalization program (PHP), if your doctor certifies that you need at least 20 hours of therapeutic services per week.
How many days do you have to stay in a hospital for Medicare?
Medicare inpatients meet the 3-day rule by staying 3 consecutive days in 1 or more hospital(s). Hospitals count the admission day but not the discharge day. Time spent in the ER or outpatient observation before admission doesn’t count toward the 3-day rule.
How many days does Medicare cover SNF?
SSA Section 1861(i) and 42 CFR Section 409.30 specify Medicare covers SNF services, if the patient has a qualifying inpatient stay in a hospital of at least 3 consecutive calendar days, starting with the calendar day of hospital admission but not counting the day of discharge.
Who recovers overpayment from SNF?
If the contractor determines the provider is at fault for the overpayment (for example, the provider didn’t exercise reasonable care in billing and knew or should have known it would cause an overpayment), then the contractor recovers the overpayment from the SNF.
Can a patient be eligible for SNF?
Patient doesn’t qualify for Medicare SNF extended care services, unless a SNF 3-Day Waiver applies. If the SNF admits the patient to a SNF for extended care services, submit a no-pay claim.