How do you write a progress note for physical therapy?
Apr 18, 2021 · 1. SOAP notes: SOAP notes are the most common type, containing four separate types of information in four distinct rows:. S = Subjective information, such as quotes from the client, or paraphrased statements they’ve given in session. It’s best to choose a few sentences that best represent the most pressing concern your client brought into the session.
Is a progress report considered a treatment note?
performing your daily tasks in Optima’s Care Operations Management. The Participant Guide provides simple, step-by-step instructions for completing tasks. We recommend that you use this guide in conjunction with the short micro-learning videos available on Optima’s YouTube channel.
What is a progress note in nursing?
©2017 Optima Healthcare Solutions Page | 9 To end the Case, follow these steps: Step Action 1. It’s important to note that all open therapy tr acks must be closed before the patient’s case can be closed. 2. From the Case Manager, click End Case. The “End Patient Case Popup” appears. 3. Specify the End Date to be used.
How often should a PT write progress report?
progress note •Within the progress note: Select the procedure code based on the service provided Enter the duration of the service Face to Face Time = time spent seeing the client Other Time = •time spent providing a service to a significant support person •time spent writing the progress note and completing other applicable forms

Is Rehab Optima easy to use?
Overall Optima is a full service, easy to use SNF therapy software program. Would like the BI support team to have a little more proactive knowledge about the dashboards. Seems like new products/dashboards are introduced in Release Notes but then minimal knowledge when questions are asked of the support team.
What is a progress note PT?
According to Mosby's medical dictionary, progress notes are “notes made by a nurse, physician, social worker, physical therapist, and other health care professionals that describe the patient's condition and the treatment given or planned.” With respect to Medicare, a progress note (a.k.a. progress report) is an ...Nov 13, 2020
How to add New patient on rehab optima?
1. From the Daily Activity Log screen, right click on the patient's name. 2. Select Add Visit.
How do you write a progress note example?
6:177:09Clinician's Corner: Writing a good progress note - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo make sure you think about that and number three make sure that when you're writing a plan it'sMoreSo make sure you think about that and number three make sure that when you're writing a plan it's very specific so again number one write a story number two remember that your diagnosis is a label.
Can a Cota write a progress note?
Nope. In all situations that we're aware of, licensed physical therapists and occupational therapists are the only providers who are able to supervise physical therapist assistants and occupational therapy assistants, respectively.Dec 4, 2019
What is Rehab Optima called now?
While there are multiple options for therapy software, there are really only two winners that have risen to the top for consideration when shopping for therapy management software within the SNF setting: Casamba and Net Health (formerly Rehab Optima).Jan 5, 2021
What documentation system does select rehab use?
PDPM Solutions | Select Rehabilitation.
When should GG tab be completed?
For an eval only that is completed at least 2 days after the facility admission, Rehab Optima will require an admission GG assessment and discharge GG assessment to be completed. For this situation enter dashes in all performance areas.
What is a progress note in therapy?
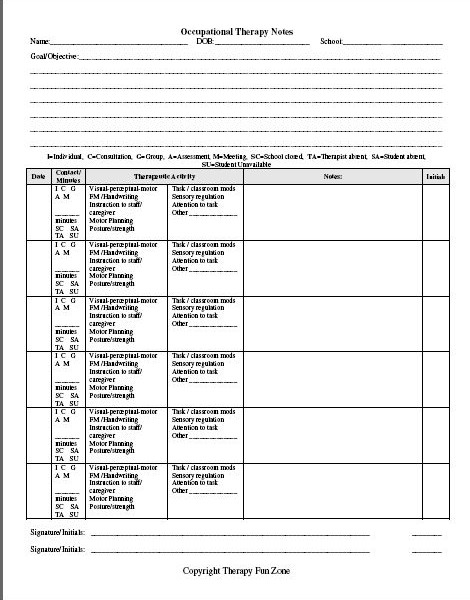
A therapy progress note updates a prescribing physician on their patient’s current status towards their rehab goals. This kind of note can also take the place of a daily note, since it follows the standard SOAP formula for daily documentation. In keeping with SOAP, a progress note typically includes the following:
What is the key word for a special test in an objective report?
It’s important to include relevant special tests in your Objective report – keyword, “relevant.”. Don’t include every possible special test; that would make it difficult for the physician to locate pertinent findings. Include only the most relevant tests and indicate whether it is a positive (+) or negative (-) finding.
Why do I become a physical therapist?
You became a physical therapist to help people move better, but part of your job involves writing documentation, such as daily notes or therapy progress notes. If you’re wondering how to write a progress note or need some templates to get you started, I have just the resources to help you out!
Why is my patient not covered for services on a specific day?
This is usually due to changes in payers or changes to the patient’s coverage. In this situation, you can set a Skip Day.
What is clear schedule?
When you are working in Projections and you want to clear the schedule, the process is simple. The Clear Schedule isn’t actually as extreme as it sound, it gives you options to clear the information you want to clear while leaving the other information in place.
Where are KX modifiers applied in Optima?
Exceptions generated from the application of KX Modifiers, appears in the patient Record on the Part B Management tab on the Exceptions & Authorizations tab.
Does COM have an auto assign feature?
That’s why COM comes with an Auto-assign feature. Auto-assign lets you assign patients to therapists in the click of a button.
What is discrepancy in therapy?
A discrepancy occurs when the projected minutes and the actual minutes are not the same. This can happen for a number of reasons. Suppose the patient was not scheduled for treatment on a certain day, but on that day, the patient was in a great deal of pain, so the therapist administered a treatment. Nothing was projected, but treatment was received. Here’s another example. The patient was scheduled for 60 minutes of therapy, but, since the patient was sick with the flu that day, she opted to skip her regularly scheduled therapy appointment. In this case, minutes were projected by no actual minutes were billed.
Where is the Physician tab in a patient record?
The Physician tab, located within the Patient Record, is the place to view, add and edit information about physicians associated with the patient’s case. The information on the Physician tab populates on documents used by your therapists.
What is a hotlist?
The Hotlist is a list of issues that require your attention. Errors that need to be resolved, missing signatures and functional limitations due are just a few examples of the items that appear on the hotlist. The items on the Hotlist are user-specific so generally, no two users will have the same items on their hotlists.
What information is needed for physical therapy?
Physical therapists, on the other hand, are solely responsible for noting the following required information: 1 assessment of patient improvement or progress toward each goal; 2 decision regarding continuation of treatment plan; and 3 any changes or additions to the patient’s therapy goals.
What is progress note?
According to Mosby’s medical dictionary, progress notes are “notes made by a nurse, physician, social worker, physical therapist, and other health care professionals that describe the patient’s condition and the treatment given or planned.”.
What is the responsibility of a physical therapist?
Physical therapists, on the other hand, are solely responsible for noting the following required information: assessment of patient improvement or progress toward each goal; decision regarding continuation of treatment plan; and. any changes or additions to the patient’s therapy goals.
What is discharge summary?
Functionally, a discharge summary (a.k.a. discharge note) is a progress note that covers the reporting period from the last progress report to the date of discharge. The discharge summary is required for each episode of outpatient therapy treatment.
What information should a therapist base on a discharge?
In the case of an unanticipated discharge (e.g., the patient stops showing up for therapy or self-discharges), the therapist may base any treatment or goal information on the previous treatment notes or the verbal reports of a PTA or other clinician. Furthermore, as this CMS document explains, “In the case of a discharge anticipated within 3 treatment days of the Progress Report, the clinician may provide objective goals which, when met, will authorize the assistant or qualified personnel to discharge the patient. In that case, the clinician should verify that the services provided prior to discharge continued to require the skills of a therapist, and services were provided or supervised by a clinician.”
Can you complete a progress report prior to a 10th visit?
You can also complete a progress report prior to the tenth visit (for example, if you know you will be unable to assess the patient personally during the tenth visit, you could complete the progress note during the ninth visit). It’s important to note, however, that the reporting period would then reset on the ninth visit, meaning the tenth visit would serve as the first session for the new 10-visit reporting period.
Why is physical therapy important?
It can also be the cause of major headaches, rushed lunch hours, and excessive typing throughout the day. Students and therapists alike have experienced difficulty locating helpful physical therapy documentation examples.
What is the problem with the left knee?
Problem Summary: Increased pain at left knee, decreased ROM of left knee, decreased strength of L LE, balance deficits in standing, difficulty with weight bearing activities, altered posture, lack of home exercise program, impaired gait form and use of assistive device.
Why are abbreviations important?
Abbreviations are obviously great because they save time—but they can make our notes cryptic (useless) to others. In the ideal world, we type the abbreviation and our smartie computer fills in the full word or phrase for us. And, for those of us who use an EMR on Google Chrome, this is exactly what can happen.
How old is Mr Peppercorn?
Mr. Peppercorn is a 46-year-old male, who presents with decreased right grip strength and range of motion, as well as persistent pain, following carpal tunnel release surgery. These deficits have a negative impact on his ability to write, type, and open his laptop and door handles. Anticipate patient may progress more slowly due to diabetes in initial weeks, but BCTOQ reflects that patient is not progressing as quickly as normal, and is at risk of falling into projected 10-30% of patients that do not have positive outcomes following carpal tunnel release. Patient will benefit from skilled OT in order to address these deficits, adhere to post-op treatment protocol, and return to work on light duty for initial four weeks.
Who are the Note Ninjas?
The Note Ninjas was founded by Nicole Trubin, MS, OTR/L and Stephanie Mayer, PT, DPT. They created their Instagram account and website to serve as resources for other clinicians and students. Their focus is to provide skilled treatment ideas and show how to support chosen interventions in your documentation. Documentation plays a vital role in patient care and can be complex. Their mission is to teach others how to continue to show skilled services and how to progress skilled intervention to avoid discharging a patient too early.
Subjective
Summary of Treatment Provided
- A progress note also reports a summary of provided treatments and the number of completed visits. This gives the physician an idea of how many visits/cancellations their patient has had as well as the types of treatments you’ve provided. Your treatments may include the following: therapeutic exercise, manual therapy, neuromuscular re-education, balance/gait training, iASTM, …
Objective: Rom, Strength, Special Tests
- It’s important to include relevant special tests in your Objective report – keyword, “relevant.” Don’t include every possible special test; that would make it difficult for the physician to locate pertinent findings. Include only the most relevant tests and indicate whether it is a positive (+) or negative (-) finding. For example: ex. Neer Impingement (-), Apprehension test (-), Drop arm (+), etc. Includi…
Assessment and Goal Status
- In this section of your progress note, the physician will want to read your overall thoughts on the patient’s progress towards their goals and how you expect to advance their treatment. Using a couple lines of space, you may write something like the following: The patient has achieved all short-term goals and is progressing well towards long-term g...
Plan
- Some therapists lump together the Assessment and Plan sections of a progress note. However, you’ll notice in my sample progress note (downloadable here), I’ve included a separate line for the Plan. Here’s a brief line you might include in the Plan section: Will continue to progress with strengthening of the shoulder, including stabilization techniques and PNF manual resistance. Re…
Physical Therapy Progress Note Examples
- You can download – for free! – my sample progress note for therapists and learn how to write a progress note quickly and efficiently. Whether you are a cash-pay physical therapist, school-based PT or OT, or an outpatient therapist, this progress note outline will save you a lot of time. If you are interested in saving even more time with your documentation, check out my Therapy Documenta…