Call a local Skilled nursing facility that does rehab and ask if they have beds available. Then tell them you are interested in inpt. rehab and they will just need to coordinate with his Dr. in getting the order. I assume if he already has home health PT his Dr. is already involved.
Full Answer
What are the eligibility requirements for inpatient rehabilitation?
care you get in an inpatient rehabilitation facility or unit (sometimes called an inpatient “rehab” facility, IRF, acute care rehabilitation center, or rehabilitation hospital). Your doctor must certify that you have a medical condition that requires intensive rehabilitation, continued medical supervision, and coordinated care that comes from your doctors and therapists working together.
How to get into a rehab facility?
Nov 08, 2019 · How to Get Into Rehab. Step 1: Make the Initial Phone Call. Most rehab centers have staff standing by and waiting for your call. When you dial the number for an addiction ... Step 2: Ask About the Cost of Treatment and Insurance Coverage. Step 3: Consider Location. Step 4: Arrive at the Facility and ...
What is inpatient rehabilitation like?
rehabilitation program. • Patient must be able to participate in an intensive therapy program i.e., 3 hours per day, 5 to 6 days per week. • Patients require two or more therapy disciplines. • Patients require at least a five-day rehab stay. • Patients have the ability to make significant functional gains as a result of an acute inpatient
Does Medicare Part a cover inpatient rehabilitation?
Mar 07, 2022 · For inpatient rehab care to be covered, your doctor needs to affirm the following are true for your medical condition: 1. It requires intensive rehab 2. It needs continued medical supervision 3. It needs coordinated care from your doctors and therapists working together
What are some CMS criteria for inpatient rehabilitation facilities?
Recently, the Centers for Medicare & Medicaid Services (CMS) advised its medical review contractors that when the current industry standard of providing in general at least 3 hours of therapy (physical therapy, occupational therapy, speech-language pathology, or prosthetics/orthotics) per day at least 5 days per week ...Dec 20, 2018
What factors need to be taken into consideration by the patient family and case manager when choosing a rehabilitation facility?
10 Tips to Help You Choose a Rehab FacilityDoes the facility offer programs specific to your needs? ... Is 24-hour care provided? ... How qualified is the staff? ... How are treatment plans developed? ... Will I be seen one on one or in a group? ... What supplemental or support services are offered during and after treatment?More items...•Dec 17, 2020
What are the CMS 13 diagnosis?
Understanding qualifying conditions for admissionStroke.Spinal cord injury.Congenital deformity.Amputation.Major multiple trauma.Fracture of femur.Brain injury.Neurological disorders.More items...
Which type of rehabilitation is very intensive?
Inpatient rehab can take place in any of these settings: A separate inpatient rehab facility (IRF). These rehab programs are usually very intense. That is why they are often called “acute rehabilitation.” Patients must be able to benefit from, and receive, at least three hours of therapy five days a week.
What questions should I ask a rehabilitation facility?
Rehabilitation success depends upon it.Is the Facility Accredited? ... Does the Facility Monitor Care Quality? ... Is the Facility Clean and Appealing? ... Does the Facility Specialize in Rehabilitation Care? ... Are Board-Certified Medical Staff Available at All Times? ... What Is the Ratio of Qualified Nurses to Patients?More items...•May 31, 2020
What factors need to be taken into consideration when choosing a rehabilitation facility?
Top 5 Things to Consider When Choosing a Rehabilitation CenterDoes the facility meet your rehabilitation needs? ... Does your health insurance cover the therapy or services you need? ... Does the facility setting work for you? ... How experienced are the Physicians, Nurses and Staff? ... What are the quality outcomes of the facility?
Which tool is administered to all patients admitted to an inpatient rehabilitation facility?
1 An Inpatient Rehabilitation Facility Patient Assessment Instrument (IRF PAI) is used to collect data that drives payment. It must be completed on admission and upon discharge of the patient from the IRF.
When Medicare runs out what happens?
Medicare will stop paying for your inpatient-related hospital costs (such as room and board) if you run out of days during your benefit period. To be eligible for a new benefit period, and additional days of inpatient coverage, you must remain out of the hospital or SNF for 60 days in a row.
What is a rehab diagnosis?
The main difference is that in rehabilitation the presenting problems are limitations in activities and the main items investigated are impairment and contextual matters, whereas in medicine the presenting problems are symptoms, and the goals are the diagnosis and treatment of the underlying disease.
What are the 3 types of rehab?
The three main types of rehabilitation therapy are occupational, physical and speech. Each form of rehabilitation serves a unique purpose in helping a person reach full recovery, but all share the ultimate goal of helping the patient return to a healthy and active lifestyle.May 23, 2018
What is palliative rehabilitation?
Palliative rehabilitation is defined as the process of helping individuals with a progressive, often advanced or incurable disease reach their physical, psychological, and social potential consistent with physiological and environmental limitations and life preferences.
What is the difference between rehab and therapy?
Rehabilitation is the process that assists a person in recovering from a serious injury, while physical therapy will help with strength, mobility and fitness.Nov 25, 2016
How to get into rehab?
Step 1: Make the Initial Phone Call. Most rehab centers have staff standing by and waiting for your call. When you dial the number for an addiction treatment facility, you’ll be connected with an admissions representative who will conduct a pre-admissions assessment and guide you through the process of entering rehab.
What is addiction treatment?
Under the Affordable Care Act, addiction treatment is one of the 10 essential services that health insurance plans must cover. Your admissions representative will help you determine what services are covered by insurance and how much you might have to pay out of pocket.
What is Amy's role in addiction?
Amy is an advocate for patient- and family-centered care. She previously participated in Moffitt Cancer Center’s patient and family advisory program and was a speaker at the Institute of Patient-and Family-Centered Care’s 2015 national conference.
What is an inpatient rehab facility?
An inpatient rehabilitation facility (inpatient “rehab” facility or IRF) Acute care rehabilitation center. Rehabilitation hospital. For inpatient rehab care to be covered, your doctor needs to affirm the following are true for your medical condition: 1. It requires intensive rehab.
How long does Medicare cover inpatient rehab?
Medicare covers inpatient rehab in a skilled nursing facility – also known as an SNF – for up to 100 days. Rehab in an SNF may be needed after an injury or procedure, like a hip or knee replacement.
What is Medicare Part A?
Published by: Medicare Made Clear. Medicare Part A covers medically necessary inpatient rehab (rehabilitation) care , which can help when you’re recovering from serious injuries, surgery or an illness. Inpatient rehab care may be provided in of the following facilities: A skilled nursing facility.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
How many reserve days can you use for Medicare?
You may use up to 60 lifetime reserve days at a per-day charge set by Medicare for days 91–150 in a benefit period. You pay 100 percent of the cost for day 150 and beyond in a benefit period. Your inpatient rehab coverage and costs may be different with a Medicare Advantage plan, and some costs may be covered if you have a Medicare supplement plan. ...
Does Medicare cover speech therapy?
Medicare will cover your rehab services (physical therapy, occupational therapy and speech-language pathology), a semi-private room, your meals, nursing services, medications and other hospital services and supplies received during your stay.
Where does rehabilitation take place?
Rehabilitation may take place in a special section of the hospital, in a skilled nursing facility, or in a separate rehabilitation facility. Although Medicare covers your care during rehabilitation, it’s not intended to be long-term care. You can learn more about Medicare and long-term care facilities here.
What to do if you have a sudden illness?
Though you don’t always have advance notice with a sudden illness or injury, it’s always a good idea to talk with your healthcare team about Medicare coverage before a procedure or inpatient stay, if you can.
Does Medicare cover rehab?
Medicare Part A covers your inpatient care in a rehabilitation facility as long as your doctor deems it medically necessary. In addition, you must receive care in a facility that’s Medicare-approved. Depending on where you receive your inpatient rehab therapy, you may need to have a qualifying 3-day hospital stay before your rehab admission.
Does Medigap cover coinsurance?
Costs with Medigap. Adding Medigap (Medicare supplement) coverage could help you pay your coinsurance and deductible costs. Some Medigap plans also offer additional lifetime reserve days (up to 365 extra days). You can search for plans in your area and compare coverage using Medicare’s plan finder tool.
Does Medicare cover knee replacement surgery?
The 3-day rule does not apply for these procedures, and Medicare will cover your inpatient rehabilitation after the surgery. These procedures can be found on Medicare’s inpatient only list. In 2018, Medicare removed total knee replacements from the inpatient only list.
Does Medicare cover inpatient rehabilitation?
Medicare covers your treatment in an inpatient rehabilitation facility as long as you meet certain guidelines.
What is medical record?
Medical records. Mental health history and any behavioral health concerns. Details of alcohol use, such as the frequency of drinking, amount regularly consumed, history of drinking, previous treatments, personal or family history of addiction, any polydrug abuse, etc. Insurance information.
Is alcohol withdrawal dangerous?
The New England Journal of Medicine ( NEJM) warns that alcohol withdrawal can be potentially life-threatening a small percentage of the time, and a medical detox program is considered the optimal method for managing difficult and potentially dangerous withdrawal symptoms.
Is alcohol addiction a treatable disease?
Fortunately, alcohol addiction is a treatable disease, and there are many options for families and loved ones to choose from to facilitate recovery. An inpatient alcohol rehab center can provide some of the highest standards of care in a stable, safe, and secure environment to promote healing and recovery. Comprehensive treatment options and ...
How long does Medicare require you to stay in the hospital?
The patient’s insurance will also play a role. Medicare requires a 3-night inpatient stay in a hospital before admission. If the senior was recently hospitalized, they may be able to use their Medicare benefit.
Does Medicaid pay for skilled nursing?
Like Medicare, they will only pay if skilled care is necessary. They don’t cover long-term care expenses. Medicaid does not pay for skilled nursing care; however, it does cover room and board for long-term care. They require what is called a “ Level Of Care ” before a patient can be admitted.
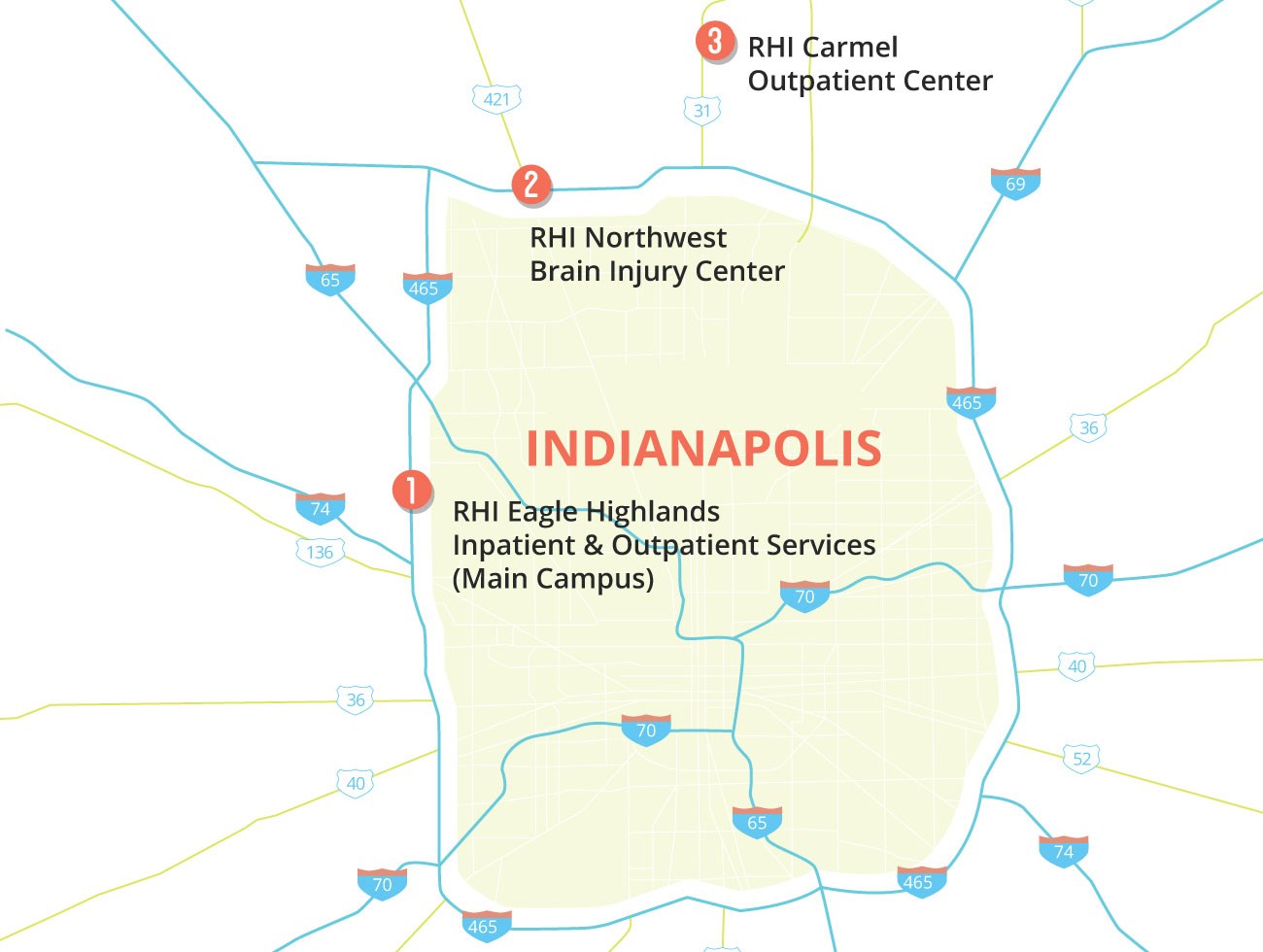
How old do you have to be to be admitted to the hospital?
Patient Requirements. For admission, patients should be: 16 years of age or older. Have a stroke, acquired brain injury, or a neurological disorder.
What are the requirements for a syringe?
For admission, patients should be: 1 16 years of age or older 2 Have a stroke, acquired brain injury, or a neurological disorder 3 Medically stable (do not require 24-hour medical care, but may have impairments in physical movement, continence, speech and language functioning, cognition, behavior, or other medical issues) 4 Level 4 or higher on the 10-level Rancho Los Amigos Scale of post-injury cognitive function