How to appeal when someone with Medicare is being discharged?
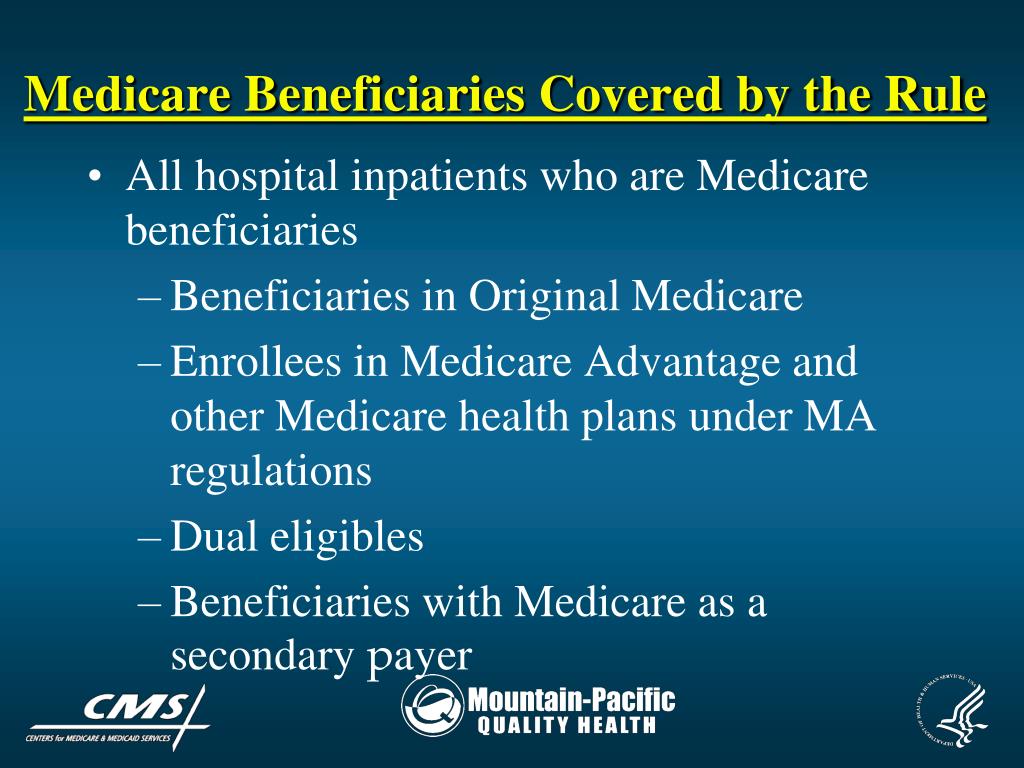
If you’re getting Medicare services from a hospital, skilled nursing facility, home health agency, comprehensive outpatient rehabilitation facility, or hospice, and you think your Medicare‑covered services are ending too soon (or that you’re being discharged too soon), you can ask for a fast appeal. Your provider will give you a notice called a Notice of Medicare Non Coverage before …
What are Medicare appeals process?
Ask the BFCC-QIO for a fast appeal no later than noon of the first day after the day before the termination date listed on your "Notice of Medicare Non-Coverage." Follow the instructions on the notice. If you miss the deadline for requesting a fast appeal from the BFCC-QIO, you can request a fast reconsideration from your plan.
What is Medicare right to appeal discharge?
Jul 04, 2016 · To implement the appeals process, the family must first inform the discharge planner that they feel the patient is being discharged prematurely and ask to file an appeal. The discharge planner cannot legally release the patient from the hospital until the process is reviewed and a decision handed down. The family must work quickly; appeals are handled …
What is Medicare appeal?
Jun 17, 2019 · Beginning June 17, 2019, CMS will accept Expressions of Interest (EOIs) for a settlement option targeted towards certain Inpatient Rehabilitation Facility (IRF) appeals pending at the Medicare Administrative Contractor (MAC), the Qualified Independent Contractor (QIC), the Office of Medicare Hearings and Appeals (OMHA) and/or Medicare Appeals Council (Council) …
How do you win a Medicare appeal?
To increase your chance of success, you may want to try the following tips: Read denial letters carefully. Every denial letter should explain the reasons Medicare or an appeals board has denied your claim. If you don't understand the letter or the reasons, call 800-MEDICARE (800-633-4227) and ask for an explanation.Nov 12, 2020
How do I write a Medicare appeal letter?
Include this information in your written request:Your name, address, and the Medicare Number on your Medicare card [JPG]The items or services for which you're requesting a reconsideration, the dates of service, and the reason(s) why you're appealing.More items...
What are the 5 levels of appeal for Medicare?
Medicare FFS has 5 appeal process levels:Level 1 - MAC Redetermination.Level 2 - Qualified Independent Contractor (QIC) Reconsideration.Level 3 - Office of Medicare Hearings and Appeals (OMHA) Disposition.Level 4 - Medicare Appeals Council (Council) Review.
How successful are Medicare appeals?
People have a strong chance of winning their Medicare appeal. According to Center, 80 percent of Medicare Part A appeals and 92 percent of Part B appeals turn out in favor of the person appealing.Jun 20, 2013
What is a Medicare appeal?
The plan must tell you, in writing, how to appeal. After you file an appeal, the plan will review its decision. Then, if your plan doesn't decide in your favor, the appeal is reviewed by an independent organization that works for Medicare, not for the plan.
How do I appeal Medicare underpayment?
You can appeal an underpayment by timely submitting a request for a redetermination appeal to your regional contractor (e.g. Palmetto-GBA for California).
What is the last level of appeal for Medicare?
The levels are: First Level of Appeal: Redetermination by a Medicare Administrative Contractor (MAC) Second Level of Appeal: Reconsideration by a Qualified Independent Contractor (QIC) Third Level of Appeal: Decision by the Office of Medicare Hearings and Appeals (OMHA)
How long does Medicare have to respond to an appeal?
The appellant (the individual filing the appeal) has 120 days from the date of receipt of the initial claim determination to file a redetermination request.Dec 1, 2021
How long does a CMS appeal take?
around 6 monthsAfter submitting your appeal you will be able to provide your supporting evidence which will be considered by a judge who will then make a decision. The appeal process usually takes around 6 months for your appeal to be heard by the tribunal.
Who pays if Medicare denies a claim?
If Medicare refuses to pay for a service under Original fee-for-service Part A or Part B, the beneficiary should receive a denial notice. The medical provider is responsible for submitting a claim to Medicare for the medical service or procedure.
What to do if Medicare denies a claim?
File your appeal within 120 days of receiving the Medicare Summary Notice (MSN) that lists the denied claim. Circle the item on your MSN that you are appealing and clearly explain why you think Medicare's decision is wrong. You can write on the MSN or attach a separate page.
How long does it take to get a notice of non-covered services?
While you're getting SNF, HHA, CORF, or hospice services, you should get a notice called "Notice of Medicare Non-Coverage" at least 2 days before covered services end. If you don't get this notice, ask for it.
What is a HHA in nursing?
You may have the right to a fast appeal if you think your services are ending too soon from one of these facilities: A Medicare-covered skilled nursing facility (SNF) A Medicare-covered. home health agency. An organization that provides home health care. (HHA) A Medicare-covered. comprehensive outpatient rehabilitation facility.
What is BCMP in Medicare?
The Beneficiary Care Management Program (BCMP) is a CMS Person and Family Engagement initiative supporting Medicare Fee-for-Service beneficiaries undergoing a discharge appeal, who are experiencing chronic medical conditions requiring lifelong care management. It serves as an enhancement to the existing beneficiary appeals process. This program is not only a resource for Medicare beneficiaries, but extends support for their family members, caregivers and providers as active participants in the provision of health care delivery.
What is a HHA?
An organization that provides home health care. (HHA) A Medicare-covered. comprehensive outpatient rehabilitation facility. A facility that provides a variety of services on an outpatient basis, including physicians' services, physical therapy, social or psychological services, and rehabilitation. (CORF)
Do you have to pay for hospice after the end of Medicare?
You won 't be responsible for paying for any SNF, HHA, CORF, or hospice services provided before the termination date on the "Notice of Medicare Non-Coverage." If you continue to get services after the coverage end date, you may have to pay for those services.
Why appeal a hospital discharge?
Appealing a hospital discharge allows the patient more time to be treated in a hospital and offers the family more time to prepare for home care or to find the right rehab facility.
How long does it take to appeal a nursing home?
An appeal can be reviewed within a one- to two-day time period. So use the time wisely. If you need to research nursing home rehab centers, start making calls and touring facilities. If the patient will be returning home, use this time to prepare the apartment properly.
What is a QIO in Medicare?
Every state has at least one Medicare Quality Improvement Organization , (QIO), that will intervene when a person appeals a hospital discharge. A QIO is a private, usually not-for-profit organization that is staffed by health care professionals who are trained to review medical care and determine if a case has merit.
What is prospective payment system?
This practice is called “the prospective payment system”. The hospital is paid the same amount no matter how long the patient stays in the hospital, which encourages the facility to discharge patients as quickly as possible.
Why do hospitals have to discharge patients?
In fact this is the standard protocol for hospitals. Hospitals are under intense pressure to discharge patients as quickly as possible after they are out of immediate danger. This is due to Medicare’s payment policy. Medicare pay hospitals a predetermined fixed amount that is tied to each patient’s diagnosis.
Can Medicare patients appeal discharge?
Fortunately, Medicare offers a safe recourse—any hospitalized patient covered by Medicare can appeal a hospital discharge. An even greater benefit is the patient can stay in the hospital during the appeal process and continue to be treated at no extra cost.
Who pays for QIO?
The QIO is paid by the federal government and not affiliated with a hospital or HMO. While the QIO is reviewing the appeal, the patient can remain in the hospital—at no cost— until a decision is made. The good news is, even If the QIO decides that patient can be discharged safely, the patient will not be responsible for paying the hospital charges ...
When is a CMS appeal pending?
Appeals must be pending at the MAC, QIC, OMHA, and/or Council, as of the date the settlement agreement is signed .
When is the last day to submit an Expression of Interest for the Inpatient Rehabilitation Facility?
September 3, 2019 - As a reminder, the last day to submit an Expression of Interest for the Inpatient Rehabilitation Facility appeals settlement option is September 17, 2019. Details about the process, including a fillable Expression of Interest Form, are available in the downloads section below. July 11, 2019 – Medicare Learning Network Provider ...
Does CMS counter sign?
CMS will counter sign and send a copy of the fully executed Agreement to the appellant. At any time prior to the appellant signing the agreement, the appellant may withdraw from the settlement process and will retain their full appeal rights.
Can an appellant choose to settle an appeal?
If an appellant is approved for participation in this process, the resulting settlement will apply to all eligible appeals from that appellant. As part of the settlement agreement, the appellant cannot choose to settle some appeals and continue to appeal others.
How long does it take for a non-covered patient to appeal a Medicare decision?
The QIO should make a decision no later than two days after your care was set to end.
What happens if you appeal a QIO discharge?
If your appeal to the QIO is unsuccessful, you will not be held responsible for the cost of the 24-hour period while you waited for the QIO to make a decision.
How long does it take to appeal a QIO denial?
You have until noon of the day following the QIO’s denial to file this appeal. The QIC should make a decision within 72 hours.
What is a QIO notice?
This notice explains in writing why your hospital care is ending and lists any Medicare coverage rules related to your case. The QIO will request copies of your medical records from the hospital.
How long does it take to get a QIC decision?
If you miss the QIC deadline, you have up to 180 days to file a standard appeal with the QIC. The QIC should make a decision within 60 days. If the appeal to the QIC is successful, you should continue to receive Medicare-covered care, as long as your doctor continues to certify it.
How long does a hospital stay notice have to be signed?
This notice explains your patient rights, and you will be asked to sign it. If your inpatient hospital stay lasts three days or longer, you should receive another copy of the same notice before you leave the hospital. This notice should arrive up to two days, and no later than four hours, before you are discharged.
How long before home health care ends should you get a notice?
You should get this notice no later than two days before your care is set to end. If you receive home health care, you should receive the notice on your second to last care visit. If you have reached the limit in your care or do not qualify for care, you do not receive this notice and you cannot appeal.
How long does a nursing home have to deliver a notice of appeal?
Remember, notice must contain all the information necessary to make it valid, and it must be delivered at least two days before ...
How long does it take for a QIC to notify you?
The QIC will notify all parties within 72 hours of its decision (usually by telephone, followed up by a letter).
Why is Mossy Mountain moving Ward?
Because Ward has a host of other health issues, Mossy Mountain is moving Ward to a general skilled nursing services bed . . . but Mossy Mountain told Mrs. Cleaver she needs to get them a check by Friday.
What should a Medicare appeal letter include?
Finally the Medicare appeal letter itself should include all relevant details. Outline the facts and dates of service and any doctor’s orders that affect your claim. Keep it professional. When Medicare or an insurance company denies a claim, we become angry or emotional.
What happens if you miss a Medicare letter?
If they get no reply, they notify Medicare and Medicare assesses a late penalty. When Medicare does this, the Part D carrier MUST comply. They must charge you the penalty – they have no choice.
How long does Medicare cover SNF?
It will cover up to 100 days in a SNF, with the goal being that the beneficiary can then resume normal self-care. Medicare Advantage plans follow these same rules. It appeared Joe was refusing to try to get well, so the carrier actually did have grounds to deny the claim.
What happened to the man who fell on his back?
The fall had caused him to break his arm and bruise his back. Upon admittance to the hospital, he was diagnosed with low blood pressure, low oxygen and a severe and debilitating UTI. This infection, coupled with the pain medication he was given, had left him feeling weak, foggy and confused.
Does Medicare pay for skilled nursing facilities?
The Medicare Advantage carrier then denied payment for the Skilled Nursing Facility (SNF). Their denial stated that Joe had “refused to participate” in therapy that would begin his rehabilitation. Medicare generally does not provide skilled nursing facility care for beneficiaries who are not expected to recover.
How long does it take for Medicare to decide on a rehab appeal?
Decisions are typically made within 72 hours, and while the appeal is pending, Medicare continues to cover rehab costs. Even if Medicare determines that the patient no longer qualifies for coverage, the patient still has a right to the bed in the rehab facility.
Can a nursing home stay in a nursing home if Medicare coverage discontinues?
In fact, a nursing home resident has the right to remain in the facility even if Medicare coverage discontinues. Being discharged early. The reasons for this vary, but in many cases nursing homes choose to discharge rehab patients based on their assessment that the patient has plateaued.
.JPG/:/rs=w:600,h:300,cg:true,m/cr=w:600,h:300/qt=q:1)