Does Medicaid pay for drug rehab for alcoholics?
Jan 31, 2022 · Length of Rehab Stay Covered by Medicaid The length of time a person spends in rehab depends on their individual needs as well as their specific provider benefits. There is no predetermined length of treatment that applies to everyone. However, evidence indicates that treatment outcomes are contingent on adequate treatment length. 10
How long does Medicare Part a cover drug rehab?
Jul 27, 2021 · Most treatment duration, however, is based on individual patient needs. [8, p15] Inpatient rehab centers typically admit residents anywhere from 15-90 days, though this too can vary based on individual needs. Treatment length is often long-term to help prevent relapse and encourage life-long sobriety.
Is drug and alcohol addiction treatment covered by insurance?
Aug 19, 2021 · Each state determines their own programs as well as the type, amount, duration, and scope of services, within federal guidelines. In most cases, Medicaid will cover most or the entire cost of drug or alcohol rehabilitation and treatment, including rehab.
How many days can you stay in a hospital for addiction?
Apr 08, 2022 · Inpatient/residential treatment centers provide drug and alcohol rehab while you live onsite at the facility. Most inpatient programs last anywhere from 15–90 days, depending on the program you’re in and your individual needs. Medicaid may cover residential treatment depending on the length of the treatment program.

How long does it take to get clean in rehab?
Most addicted individuals need at least three months in treatment to get sober and initiate a plan for continued recovery. Research shows that the best outcomes occur with longer durations of treatment.Nov 4, 2021
What is the average time spent in rehab?
Many treatment facilities typically offer patients short-term stays between 28 to 30 days. However, certain residential facilities may also offer extended stays for an additional fee, provided the patient is showing positive signs of recovery.Feb 2, 2022
What are the 5 stages of rehab?
Don't Forget the RehabPhase 1 - Control Pain and Swelling.Phase 2 - Improve Range of Motion and/or Flexibility.Phase 3 - Improve Strength & Begin Proprioception/Balance Training.Phase 4 - Proprioception/Balance Training & Sport-Specific Training.Phase 5 - Gradual Return to Full Activity.
Does Wisconsin Medicaid cover residential treatment?
Since 2017, Wisconsin's Medicaid program has covered residential substance use disorder treatment on a limited basis through the Comprehensive Community Services program, allowing treatment in smaller facilities with 16 or fewer beds.Jan 29, 2021
What rehab has the highest success rate?
Roughly 80 percent of patients report benefiting from improved quality of life and health after completing drug and alcohol rehab. Florida has the highest success rates of drug rehab compared to all other states.May 29, 2019
How long does rehab last after stroke?
The rate of recovery is generally greatest in the weeks and months after a stroke. However, there is evidence that performance can improve even 12 to 18 months after a stroke.
What are the 3 P's of recovery?
3 “P's” for Recovery: Passion, Power and Purpose.Aug 18, 2016
What are the 3 phases of rehab?
Athletic trainers (ATs) have traditionally conceptualized rehabilitation programs in terms of 3 distinct physiologic phases: acute injury phase, repair phase, and remodeling phase.
How long does the subacute phase last?
The care of acute (and recurring acute) injuries is often divided into 3 stages with general time frames: acute (0–4 days), subacute (5–14 days), and postacute (after 14 days).
Finding Medicaid covered Drug Rehab Centers Near Me
Yes, Medicaid does provide some coverage for drug and alcohol addiction rehab, though the amount of the cost covered varies from state to state and depends on an individual’s income and need for treatment. 1 Medicaid is a government-funded insurance program for low-income individuals.
Does Medicaid cover Substance Abuse Treatment?
Medicaid is the largest payer for substance use disorder treatment and recovery services in the United States. 3 If you are seeking drug addiction treatment and have Medicaid health insurance, you are not alone.
How many days does Medicaid pay for rehab?
The length of time Medicaid covers rehab varies. Generally, Medicaid has limits on the amount of coverage per year in categories of treatment. For example, inpatient treatment duration may be limited to a certain number of days per calendar year. Most treatment duration, however, is based on individual patient needs. [8, p15]
Who qualifies for Medicaid?
Medicaid is a government-funded public insurance program for low-income individuals and families. Medicaid covers some aspects of drug and alcohol dependency treatment.
Medicaid Sponsored Alcohol and Drug Rehab Centers
Looking for an affordable rehab center can be frustrating and exhausting. However, the process can be pretty straightforward as long as you are well-informed and know where to seek out information. The important thing to keep in mind is that Medicaid can help you reduce or even eliminate the cost of drug and alcohol addiction treatment.
How to Check Your Medicaid Coverage for Addiction Treatment?
American Addiction Centers can help you determine what is covered by Medicaid and assist you in speaking to relatives about financing any out-of-pocket treatment expenses. Give us a call at (888) 287-0471 Helpline Information to speak with one of our admissions navigators. We are happy to help.
What is Medicaid for drug rehab?
Medicaid for Drug and Alcohol Rehab. Medicaid is the single largest payer for mental health and substance abuse in the United States. The Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008 is a federal law that requires coverage for mental health and substance use disorders to be no more restrictive than coverage ...
What is Medicaid insurance?
Medicaid is a public health insurance program that provides eligible individuals access to certain health care services. It is administered by each state independently along with assistance from the federal government. Each state determines their own programs as well as the type, amount, duration, and scope of services, within federal guidelines.
What is the largest payer for mental health?
Medicaid is the single largest payer for mental health and substance abuse in the United States. The Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008 is a federal law that requires coverage for mental health and substance use disorders to be no more restrictive than coverage that is generally available for other medical conditions. This applies to: 1 Copays, coinsurance, and out-of-pocket maximums 2 Limitations of services utilization (ex: limits on the number of inpatient days or outpatient visits that are covered) 3 Use of care management tools 4 Criteria for medical necessity determinations
How long does it take to get a disability insurance plan?
States have 45 days to process an application and 90 days if the eligibility is in relation to a disability. Those who don’t qualify may be eligible for a subsidized plan through the federal Marketplace during open enrollment.
How old do you have to be to get medicaid?
In order to be eligible for Medicaid, those who apply must be one of the following and make less than 100-200% of the federal poverty level (FPL): Over 65 years old.
Does Medicaid cover addiction treatment?
Figuring out how to pay for addiction treatment can be frustrating and complicated. Medicaid can help cover the cost of services such as detox, medication, and rehabilitation. Contact a treatment provider for more information.
What is Medicaid for drug rehab?
Medicaid for Drug and Alcohol Rehab. Medicaid is a public insurance program for low-income families. Under the 2010 Affordable Care Act (ACA), also known as “Obamacare,” insurance providers (including Medicaid) must cover all basic aspects of drug and alcohol dependency recovery. While Medicaid covers substance abuse treatment, ...
How long does Medicare cover inpatient rehabilitation?
Part A covers up to 60 days in treatment without a co-insurance payment. People using Part A do have to pay a deductible. Medicare only covers 190 days of inpatient care for a person’s lifetime. Part B.
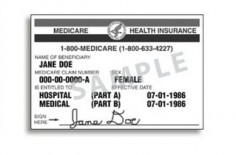
What is the most commonly used method for paying for drug and alcohol rehab?
What Are Medicaid and Medicare? Some of the most commonly used methods for paying for drug and alcohol rehab, Medicaid and Medicare are federal- and state-funded health insurance programs. These insurance programs can provide free or low-cost drug and alcohol addiction treatment.
How old do you have to be to get medicaid?
Medicaid Eligibility by Income. To be eligible for Medicaid, applicants must be one of the following: Over 65 years old. Under 19 years old. Pregnant. A parent. Within a specified income bracket. In some states, Medicaid covers all adults below a certain income level.
What is the poverty level for Medicaid?
The ACA requires people to earn less than 133 percent of the federal poverty level (FPL) to be eligible for Medicaid. A person living above the poverty level may still be eligible for government insurance if they fall in the right income bracket.
Does Medicare cover drug rehab?
Medicare can cover the costs of inpatient and outpatient drug rehabilitation. It consists of four parts that cover different parts of addiction recovery programs. Insurance for Hospital Stays. Medicare Part A can help pay for inpatient rehabilitation.
Does Medicare cover substance abuse?
Medicare and Medicaid may cover part or all of your substance abuse treatment costs. Every state has different rules for eligibility and treatment coverage. Rules for eligibility also change annually. If you were turned down for Medicaid or Medicare in the past, you could be eligible now.
What is Medicaid?
Medicaid is a federal- and state-funded program that provides healthcare coverage to people who meet its income and other eligibility requirements. In most cases, you must qualify for Medicaid based on Modified Adjusted Gross Income (MAGI). 3 This method determines Medicaid eligibility for children, pregnant women, and adults.
Does Medicaid Cover Addiction Treatment?
Medicaid typically pays at least some part of drug and alcohol rehab treatment. State insurance does typically cover rehab for most individuals. While Medicaid does often cover substance abuse treatment, Medicaid addiction treatment coverage is also highly dependent on individual state policies.
Types of Substance Abuse Treatment That Medicaid Covers
With most Medicaid plans covering at least some of the costs of rehab treatment for drug and alcohol addiction, the types of treatment can vary in intensity and frequency. Types of treatment may include: 6,7
How to Check Your Medicaid Rehab Coverage
Before choosing the right addiction treatment center for you, check your Medicaid policy benefits to determine which costs will be covered by your insurance company and which will be out-of-pocket for you.
Rehab Centers That Accept Medicaid
In most cases, you will need to seek drug and alcohol treatment at a rehab facility that is in-network with Medicaid to receive your full benefits. Even if you choose a treatment center that is in-network, you may still be responsible for some of the treatment costs.
How long does rehab last in a skilled nursing facility?
When you enter a skilled nursing facility, your stay (including any rehab services) will typically be covered in full for the first 20 days of each benefit period (after you meet your Medicare Part A deductible). Days 21 to 100 of your stay will require a coinsurance ...
How long do you have to be out of the hospital to get a deductible?
When you have been out of the hospital for 60 days in a row, your benefit period ends and your Part A deductible will reset the next time you are admitted.
How long does Medicare cover SNF?
After day 100 of an inpatient SNF stay, you are responsible for all costs. Medicare Part A will also cover 90 days of inpatient hospital rehab with some coinsurance costs after you meet your Part A deductible. Beginning on day 91, you will begin to tap into your “lifetime reserve days.".
How much is Medicare Part A deductible for 2021?
In 2021, the Medicare Part A deductible is $1,484 per benefit period. A benefit period begins the day you are admitted to the hospital. Once you have reached the deductible, Medicare will then cover your stay in full for the first 60 days. You could potentially experience more than one benefit period in a year.
How much is coinsurance for inpatient care in 2021?
If you continue receiving inpatient care after 60 days, you will be responsible for a coinsurance payment of $371 per day (in 2021) until day 90. Beginning on day 91, you will begin to tap into your “lifetime reserve days,” for which a daily coinsurance of $742 is required in 2021. You have a total of 60 lifetime reserve days.
What day do you get your lifetime reserve days?
Beginning on day 91 , you will begin to tap into your “lifetime reserve days.". You may have to undergo some rehab in a hospital after a surgery, injury, stroke or other medical event. The rehab may take place in a designated section of a hospital or in a stand-alone rehabilitation facility. Medicare Part A provides coverage for inpatient care ...
Does Medicare cover outpatient treatment?
Medicare Part B may cover outpatient treatment services as part of a partial hospitalization program (PHP), if your doctor certifies that you need at least 20 hours of therapeutic services per week.
What is Medicare for rehab?
Medicare if a federal health insurance program that help people over the age of 65 afford quality healthcare. Find out about eligibility and how Medicare can help make the cost of rehab more affordable.
What is the Medicare number for substance use disorder?
If you’re battling a SUD or an AUD and qualify for Medicare benefits, please reach out to one of our admissions navigators at. (888) 966-8152.
What is long term care?
Inpatient care as part of a qualifying research study. Mental health care. An inpatient drug and alcohol rehabilitation program, combined with follow-up care and support, can support a person struggling with addiction to attain long-term recovery.
How long can you be in hospice?
Part A will cover inpatient care for a substance abuse disorder if the services are determined to be reasonable and necessary. 5. Under Part A, an individual can complete no more than 190 days total treatment from a specialty psychiatric hospital. This is the lifetime limit.
How old do you have to be to qualify for Medicare?
You may be eligible for Medicare if: 1. You are age 65 or older. You are younger than 65 and have a disability. You are younger than 65 and have end stage renal disease (permanent kidney failure that requires dialysis or a transplant).
How many hours of treatment is required for partial hospitalization?
A physician must certify that individuals in partial hospitalization require that form of treatment, and the person’s plan of care must include at least 20 hours of treatment per week. 5. Services offered in partial hospitalization programs include: 5. Individual and group therapy. Occupational therapy.
Is addiction covered by Medicare?
But there are rules about the providers people can use with Medicare, and some types of addiction treatment are not covered by Medicare at all. It is a good idea to contact the Medicare organization directly to find more detailed information. You are age 65 or older.
How much does Medicare pay for substance abuse?
Medicare. Medicare Advantage. Substance abuse costs the US more than $740 billion every year. Those costs are related to crime, healthcare, and lost productivity at work. Overcoming addiction is a lot of work, and it takes a team of mental health and medical professionals to keep you on the right path. You might know that Medicare will pay ...
What is the level of care for addiction?
The American Society of Addiction Medicine (ASAM) divides treatment into five levels of care. Here’s how they relate to Medicare: Level 0.5, Early Intervention. Education and prevention for people who are at risk of developing an addiction fall under this level.
What percentage of older adults have an addiction problem?
The percentage of older adults who met the criteria for having an addiction problem was 11.7 percent.
How to contact SAMHSA?
You reach the helpline at 1-800-662-HELP (4357) or use SAMHSA’s online treatment finder tools.
Does Medicare cover alcohol rehab?
Medicare does cover many of the costs related to alcohol rehab and treatment if your provider says those services are medically necessary. You must get treatment at a Medicare-approved facility or from a Medicare-approved provider, and that provider must create a care plan.
Does Medicare pay for alcohol and substance abuse?
It starts small, often with preventive measures, and will progress according to the doctor’s recommendations. Medicare pays for alcohol and substance abuse treatment for both inpatients and outpatients. Substance use disorders are drug addictions that influence a person’s thoughts, feelings, and behaviors.
Can you face drug addiction alone?
If you or someone you love struggles with drug or alcohol addiction, you don’t have to face it alone. A licensed agent with Medicare Plan Finder may be able to help you find a Medicare plan with the right care team to lead your or your loved one’s recovery.
When did California become the first state to restructure substance abuse treatment?
In 2015, California became the first state in the nation to receive federal permission to restructure substance abuse treatment for Medicaid beneficiaries, a move which has made these life-changing services more widely accessible to the over 13 million Californians who receive Medi-Cal, California’s Medicaid program.
What is a medicare program?
is a public health insurance program which provides needed health care services for low-income individuals including families with children, seniors, persons with disabilities, fost er care, pregnant women, and low income people with specific diseases such as tuberculosis, breast cancer or HIV/AIDS . Those eligible for Medi-Cal also include ...
What is the importance of inpatient treatment?
An addiction can cause a state of upheaval in an individual’s life, and the stability and security inpatient treatment offers supports the healing and personal growth which are foundational to a solid recovery.
What is Medi-Cal in California?
Medi-Cal, California’s Medicaid program, offers health care services for the treatment of substance use disorders. This assistance may help you to obtain outpatient, residential, and opioid treatment program services, among others.
What is the number to call for a SUD waiver?
Call Now: (888) 407-2072. One of the main goals of this waiver is to provide Medi-Cal beneficiaries with a “continuum of care for substance use disorder treatment services” which are based upon those established by the American Society of Addiction Medicine (ASAM) Criteria for SUD treatment services.
What does it mean when a substance abuse disorder must be documented?
This means that the substance use disorder must be documented and also that evidence is provided which illustrates that substance abuse treatment is necessary in order for a person to get well. To determine this a substance abuse assessment will likely be conducted.
Does Medi-Cal offer opioid treatment?
Opioid addictions caused by heroin and prescription painkillers are often those which necessitate this care. Medi-Cal does offer opioid or narcotic treatment program services; for some individuals this care may be offered through a residential inpatient drug rehabilitation program. For these individuals, medication-assisted treatment (MAT), ...