How long does Medicare pay for inpatient rehab?
Summary of Benefits and Coverage: What this Plan Covers & What You Pay For Covered Services Coverage Period: 01/01/2022-12/31/2022 CDPHP UBI: FEHB Standard Option Coverage for: Self Only, Self Plus One or Self and Family | Plan Type: Federal EPO 1 of 6 The Summary of Benefits and Coverage (SBC) document will help you choose a health plan.
Do New York treatment centers accept CDPHP insurance?
You have the option to pay by credit card or eCheck. Enter the required information and click Continue. Or, you can mail your payment to the following address. Please allow seven to 10 business days to ensure that your check is received and processed by the due date. CDPHP PO BOX 5525 Binghamton, NY 13902-5525. Additional Online Payment Information
How long does it take to receive a CDPHP check?
Dec 07, 2021 · Medicare Part A covers 100 days in a skilled nursing facility with some coinsurance costs. After day 100 of an inpatient SNF stay, you are responsible for all costs. Medicare Part A will also cover 90 days of inpatient hospital rehab with some coinsurance costs after you meet your Part A deductible. Beginning on day 91, you will begin to tap into your …
How do I pay my CDPHP Bill?
Rehabilitation $15 services co-pay /visit Not Covered Up to 60 visits are covered per condition per lifetime. Habilitation services $15 co-pay /visit Not Covered Limited to coverage for Applied Behavioral Analysis when necessary for the treatment of Autism Spectrum Disorder. All contract limits and provisions for managed benefits apply.

What is Granite Recovery Center?
"Granite Recovery Centers is dedicated to providing high quality, affordable addiction treatment. At GRC we offer individuals struggling with addiction, a full spectrum of care from medical detoxification and primary residential treatment to extended care, Intensive outpatient, and sober living. Each of our premier treatment programs has a specific location and focus; however, all of our programs are deeply rooted in the 12 step principals and traditions. We understand the relationship between addiction and mental health. We have highly-trained clinical teams of experts at each of our centers that are there to assist those struggling with co-occurring disorders. We work with most insurances and Green Mountain Treatment Center is in Network with Blue Cross and OPTUM. OPTUM plans include: Harvard Pilgrim Healthcare, United Behavioral Healthcare, United Healthcare, Health Plans Inc., and OPTUM. Our admissions team is always available to answer any questions."
What is Gatehouse Treatment?
"Gatehouse Treatment is a private facility providing intervention and treatment services to chemically dependent persons and individuals with co-occurring mental health issues. We offer treatment in a serene, luxurious setting, and our staff has decades of experience treating substance abuse and dual diagnosis clients. We provide individualized treatment in a small, gender specific environment. Also, Gatehouse offers one the only comprehensive vocational program in New England which allows our clients to enroll or re-enroll in college or trade school, obtain a job in the career of their choice, and manage debt and legal problems. At Gatehouse, evidence-based practice is applied along with creative and cutting-edge interventions. We provide extraordinary care and enable our clients to gain insight into their underlying factors driving addictive and co-dependent behaviors, set realistic goals and dramatically improve their chances of Achieving long-term recovery and fulfilling productive and fruitful lives."
What is Mountainside Recovery?
"Having helped thousands of individuals suffering with substance abuse and alcoholism, Mountainside is the foremost comprehensive, innovative addiction rehabilitation treatment center in the Northeast. Our mission is to elevate the standard in comprehensive drug and alcoholism addiction treatment in order to provide an unequaled rehabilitation experience for our clients."
What is Miramar Recovery?
"Miramar Recovery is an exclusive, highly experienced treatment facility that can help you towards successful and lasting healing from substance abuse. No matter how miserable and isolated your addiction may make you feel, you are not alone. We absolutely can help you. Our uniquely qualified and experienced team of professional substance abuse treatment experts knows from their own personal experience and/or that of immediate family members what you are experiencing. You need a team of professionals, who can relate to you and your specific issues. We do this with absolute integrity and expertise. We treat the entire spectrum of alcohol and drug addiction and their accompanying underlying mental illnesses. Please don't continue to suffer! Get the help and care you need and deserve in a safe, confidential, and highly supportive environment. Call now to start healing."
What is an addiction center?
"American Addiction Centers is a national behavioral healthcare provider focused on addiction treatment and rehabilitation. Our staff, which includes expert drug addiction specialists, seasoned physicians and caring therapists, is dedicated to providing our patients with the absolute best, proven methods of treatment and rehabilitation. Our facilities, located across the country, offer unmatched integrated programs and services that honor mind, body and soul. Effective addiction recovery incorporates comprehensive treatment focused on uncovering and addressing the roots of addiction. Whether it's in our initial clinical assessments, medically supervised detox, residential rehabilitation or aftercare, our team is present for and committed to each step of the recovery process for every individual. We welcome you to explore American Addiction Centers, where you can find hope today."
What is the Medicare therapy cap?
The Medicare therapy cap was a set limit on how much Original Medicare would pay for outpatient therapy in a year. Once that limit was reached, you had to request additional coverage through an exception in order to continue getting covered services. However, by law, the therapy cap was removed entirely by 2019.
What is an ABN for a physical therapist?
This is true for physical therapy, speech-language pathology and occupational therapy. This notice is called an Advance Beneficiary Notice of Noncoverage (ABN). If your provider gives you an ABN, you may agree to pay for the services that aren’t medically necessary. However, Medicare will not help cover the cost.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
Does Medicare Advantage cover rehab?
Your costs for Medicare rehab coverage with a Medicare Advantage plan (Part C) depend on the specific plan you have. Medicare Advantage plans are offered by private insurance companies and approved by Medicare. These plans must provide coverage at least as good as what’s provided by Original Medicare (Parts A & B).
Does Medicare pay for outpatient therapy?
Technically, no. There is no limit on what Medicare will pay for outpatient therapy, but after your total costs reach a certain amount, your provider must confirm that your therapy is medically necessary in order for Medicare to cover it.1.
What is a CDPHP treatment center?
They include CDPHP Treatment Centers in New York, CDPHP psychologists and CDPHP counseling. A New York Treatment Center who accepts CDPHP, may be in network with CDPHP, or can assist you to make a claim on your CDPHP insurance (as an out of network CDPHP provider).
What is Mountainside Recovery?
"Having helped thousands of individuals suffering with substance abuse and alcoholism, Mountainside is the foremost comprehensive, innovative addiction rehabilitation treatment center in the Northeast. Our mission is to elevate the standard in comprehensive drug and alcoholism addiction treatment in order to provide an unequaled rehabilitation experience for our clients."
What are the reasons for Dean Hope Center?
"Stress due to a personal or career issue? Feelings of sadness or anxiety? Trouble making important decisions in your life ? Family or relationship conflicts? Loss of a significant loved one? Health problems? If so, the Dean Hope Center may be able to help you."
Where is IHI therapy center?
"Struggling with life? WE CAN HELP. IHI Therapy Center is New York's leading LGBTQ affirmative psychotherapy and training center. Located in the heart of Chelsea, we foster personal growth, free of traditional gender, sexual orientation or cultural bias."
How long does a POC last?
The physician’s/NPP’s signature and date on a correctly written POC (with or without an order) satisfies the certification requirement for the duration of the POC or 90 calendar days from the date of the initial treatment, whichever is less. Include the initial evaluation indicating the treatment need in the POC.
What is a POC in rehabilitation?
Outpatient rehabilitation therapy services must relate directly and specifically to a written treatment plan (also known as the POC). You must establish the treatment plan/POC before treatment begins, with some exceptions. CMS considers the treatment plan/POC established when it is developed (written or dictated) by a PT, an OT, an SLP, a physician, or an NPP. Only a physician may establish a POC in a Comprehensive Outpatient Rehabilitation Facility (CORF).
How often do you need to recertify a POC?
Sign the recertification, documenting the need for continued or modified therapy whenever a significant POC modification becomes evident or at least every 90 days after the treatment starts. Complete recertification sooner when the duration of the plan is less than 90 days, unless a certification delay occurs. CMS allows delayed certification when the physician/NPP completes certification and includes a delay reason. CMS accepts certifications without justification up to 30 days after the due date. Recertification is timely when dated during the duration of the initial POC or within 90 calendar days of the initial treatment under that plan, whichever is less.
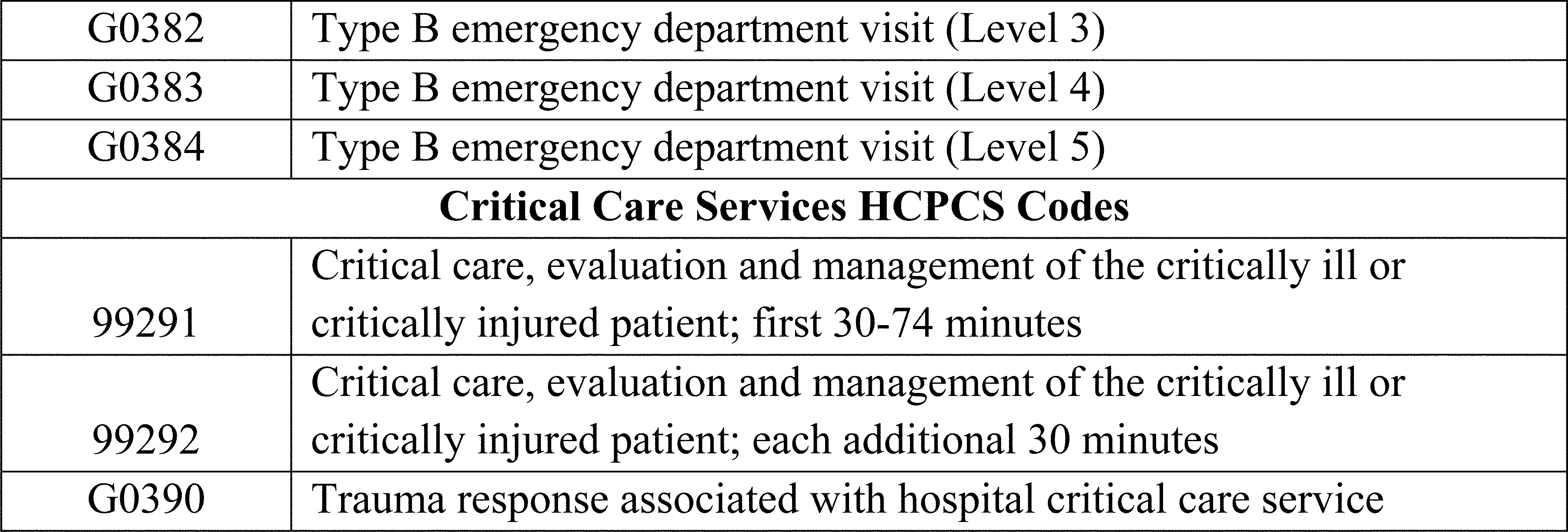
How long does a HCPCS code have to be in a day?
CMS requires that when you provide only one 15-minute timed HCPCS code in a day, that you do not bill that service if performed for less than 8 minutes. When providing more than one unit of service, the initial and subsequent service must each total at least 15 minutes, and the last unit may count as a full unit of service if it includes at least 8 minutes of additional services. Do not count all treatment minutes in a day to one HCPCS code if more than 15 minutes of one or more other codes are furnished.